It is well documented that there are 3 million people in the UK who are malnourished or at risk of malnourishment, and 93% of these individuals are in the community (BAPEN, 2018). The cost of malnutrition in England alone is estimated to be £19 billion per annum. Therefore, its early identification and management has the potential to improve quality of life and reduce the burden of spending in the NHS (Managing Adult Malnutrition, 2017). Malnutrition screening using a Malnutrition Universal Screening Tool (MUST) has long been the gold standard in identifying malnutrition (BAPEN, 2003; National Institute for Health and Care Excellence (NICE) 2012; Murphy et al 2018; Dera and Woodham, 2016). This tool is generally focused on screening patients in a hospital setting, and the actions and care plans are not appropriate for monitoring generally well patients. For example, screening in the community is needed only monthly or annually, whereas the recommendations for in an acute hospital setting are weekly screening.
The Buckinghamshire Adult Community Healthcare Team is part of the integrated Buckinghamshire Acute Community Health Trust (ACHT) and covers seven localities spread across the county. The district nursing teams make approximately 800–900 visits a day. There are approximately 300 patients in the community receiving home enteral nutrition support, although only a small percentage (>10%) require input and management from the district nursing team. The team was experiencing some issues with competency, training and confidence in home enteral feeding management and troubleshooting. Following an incident involving a patient receiving home enteral feeding via a gastrostomy tube, it was identified that there was a deficit in nurses' knowledge and competence in this area. The team involved in the incident had received input and support following the incident, but there were still issues of confidence and competence. The incident resulted in an investigation by the trust, and an action plan was agreed.
Community nutrition nurse specialist
In May 2018, the ACHT decided to appoint a community nutrition nurse specialist to work with the district nursing teams. The role (0.6 working time equivalent) was envisaged to support the district nursing team with issues surrounding home enteral feeding and nutrition screening. This was a new and innovative role, and while the appointment was to the ACHT, it was expected that the post holder would work collaboratively with community, hospital, dietitians and industry home care nurses who undertook day-to-day management of home enteral feeding.
While the role was initially designed to focus mainly on home enteral feeding issues, it was quickly identified that this would not require a significant time input on a weekly basis. The role was also designed to support nutritional screening, and this aspect was identified by the post holder to be the area that would require more focused support.
Following discussions with the clinical lead nurse for community, it was decided that the role would focus on developing a plan to address both areas, with a greater focus on nutritional screening.
Development of the community MUST
In Buckinghamshire, community MUST screening was being undertaken by the district nursing teams using a non-validated tool. The consequences of this were that patients were potentially being mis-scored. This mainly arose from the lack of options within the tool for the clinician to use a subjective score where there were other contributing factors. For instance, a review by the community nutrition nurse found that one patient's score did not reflect the nature of her illness. This patient had a cancer diagnosis and had a large pressure ulcer that was being managed by the team. Her MUST risk, as determined when MUST was used objectively, was medium, with a score of 1. The patient's body mass index (BMI) was in the normal range, and she had not lost weight recently. However, subjective assessment using MUST screening, which took into consideration the cancer diagnosis and pressure ulcer, indicated that the patient was at high risk of malnutrition.
When the screening tool was being used by the senior district nursing team, it was more likely that they would use their experience and tacit knowledge to ensure that the risk score reflected the patient status. However, junior nurses and support staff were probably less able to determine clinical risk and would tend to use the tool in isolation.
To address the situation, the community nutrition nurse started the process of redesigning the community screening tool and, subsequently, a pathway for this. The process was anticipated to be completed within 4–6 months.
To ensure that the tool met the needs of the community, the clinical lead nurse for community and the community nutrition nurse specialist worked collaboratively, involving stakeholders and partners (the clinical commissioning group's (CCG) prescribing dietitian, community dietitians and the nutritional lead nurse for the hospital). The community nutrition nurse specialist undertook a search of nationally available community-based screening tools and prepared the first draft. An additional eight versions were discussed and modified until a final version was agreed. This final version was sent to the Malnutrition Advisory Group (MAG), and they granted permission to have the tool endorsed with the BAPEN badge (Appendix 1).
When discussing screening tools, Herman (2006) advocated the need for them to have the following features:
While this tool was not designed to detect disease, it did detect malnutrition, which could be disease-related.
Once the final version was agreed, the tool was piloted for a short period in one of the localities, and feedback was sought from the teams. The feedback did not indicate that any further changes were needed. However, once in practice, a few issues were identified with the use of the tool, which were overcome through training and extra resources. Initially, the nursing teams felt that the new tool took more time to complete, and some of the teams were unsure exactly how to interpret alternative measurements, such as mid-upper arm circumference (MUAC), in relation to BMI. Additionally, the tool did not have a copy of the BMI chart, MUAC conversion chart or weight loss chart attached.
The nutrition nurse devised an A4 double-sided chart that had the BMI chart, MUAC conversion and weight loss calculator chart. This was then emailed to all the staff, who saved the document on their devices, making it easy for them to refer to these charts when calculating malnutrition risk.
During the implementation phase, the nutrition nurse was available at the bases at set times for consultation and guidance. Further, industry-related aids, such as MUAC tapes and How to screen using MUST booklets were sourced for every member of the team.
Alongside the community MUST, a pathway was developed in collaboration with the CCG (Figure 1), and both the MUST screening tool and pathway were approved and endorsed by the trust's Nursing, Midwifery and Therapy Professional Board and the CCG's Medicines Management Committee.
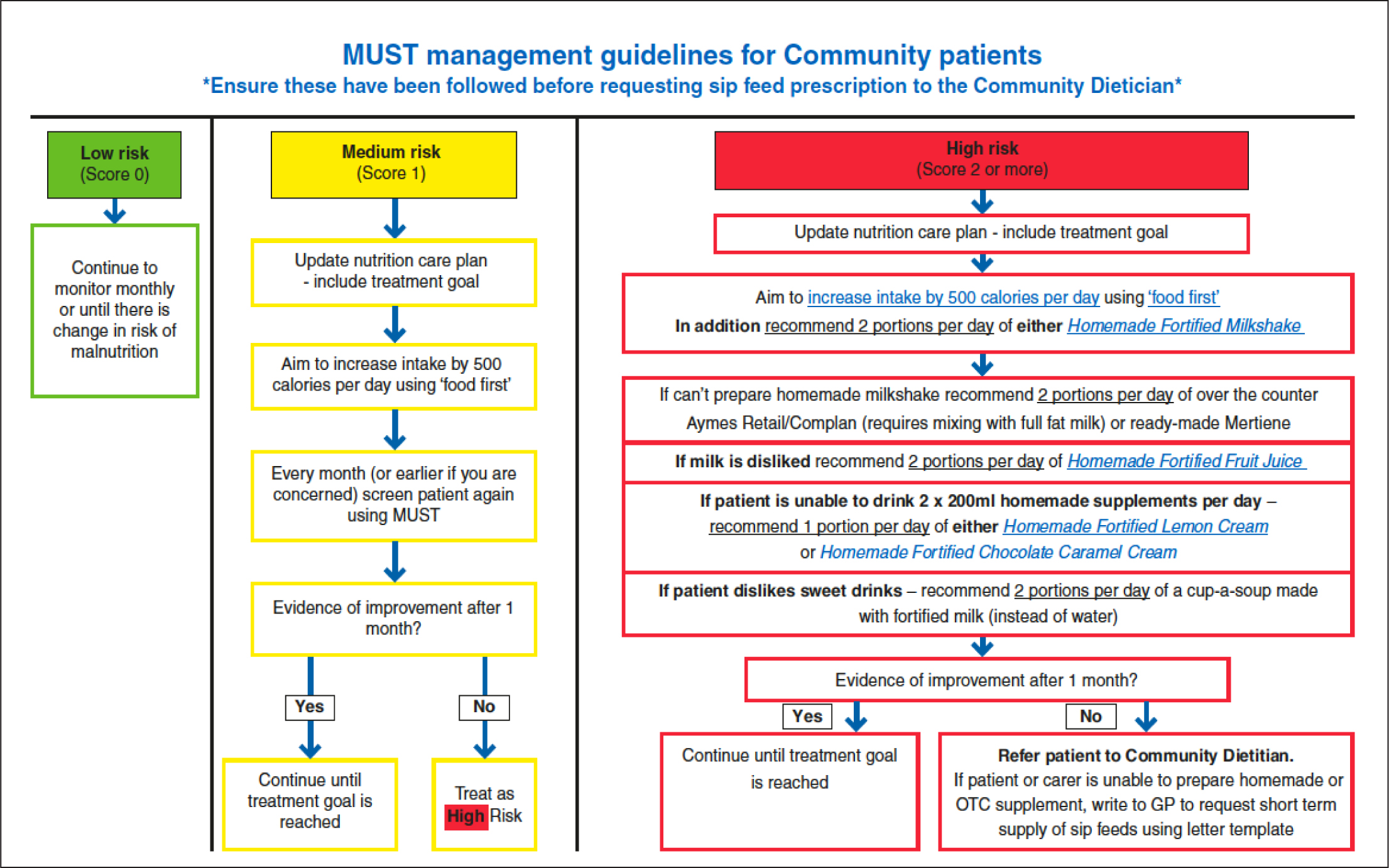
To support community staff in making effective decisions, a standard template referral letter for GPs was agreed. The aim of this was to reduce delays in the prescribing of oral nutritional supplements (ONSs). There were some initial concerns from the CCG's Medicines Management Committee regarding the potential for increased spend on ONSs, and it was agreed that this would not be fully implemented until an audit on the impact had been undertaken.
The community MUST screening tool was designed to incorporate the guidance provided in the malnutrition pathway document and supporting advice leaflets (www.malnutritionpathway.co.uk) (Managing Adult Nutrition, 2017). The guidance document provides clear directions on how to address malnutrition in the community. There were some challenges from commissioners about the validity of the work and the composition of the working party, but there was wide representation on the working group. There were also concerns expressed about the potential to increase the spending on ONSs if robust constraints were not in place. To address the issue of potential increased spend, the community dietitians agreed to monitor the number of referrals requesting ONSs to determine if there was a dramatic increase. Thus far, there has not been a considerable rise in referrals, due to the nursing teams having a better understanding of nutritional advice and the pathway. It was also agreed that an audit would be undertaken to ensure compliance with the pathway after it had been in place for 9–12 months.
The post in practice
Confidence building
One of the early priorities identified by the community nutrition nurse specialist was how to ensure all the community teams had the knowledge and confidence to screen for malnutrition. It was also identified that there was confusion about when to refer to the community dietetics team. There were many anecdotal comments about not being sure how to screen and how to use alternative methods. Stuart (2018) reported that gaps in professional training in healthcare professionals could lead to delays in appropriate treatments. Parsons (2011) also discussed the importance of nutritional screening using the MUST and reported that, although there is a high proportion of people in the community who are at risk of being malnourished, only 10% of GPs using a screening tool to determine this proportion. Given this scenario, it was vital that the district nursing teams were able to support their cohort of patients effectively.
The community dietetics team expects that, before a referral is made to them, patients are offered food first and food fortification advice and the results of this are monitored. While some of the district nursing teams were confident to do this, some expressed uncertainty in implementing this process.
To quantify the confidence of the district nursing teams in following this process, they were sent an anonymised questionnaire that only identified their team and band. The response rate was only approximately 19%, although this was better than expected. The results showed that most responders felt they had sufficient knowledge but lacked the confidence to share this knowledge. On the basis of the results of the questionnaire, the community nutrition nurse specialist developed a teaching plan and rolled this out across the county. Buckinghamshire is a very diverse county, so the teaching sessions were delivered in different localities to ensure maximum attendance. The teaching focused primarily on the importance of identifying and treating malnutrition caused by under-eating and disease. While there is a cohort of the population that potentially has obesity-associated malnourished, addressing this is beyond the remit of the community nutrition specialist nurse at this time. Any issues identified with obesity-related malnutrition are referred on to community dietitians for management.
Alongside the teaching programme, a number of resources were sourced and developed to support staff in clinical practice. The aim of this process was to increase compliance and the consistency of screening undertaken by the staff. The emphasis was not only early detection but also care planning and monitoring.
Each of the locality teams was provided with an identical resource folder containing all the relevant information, guidelines and policies. Any new information was sent to the nutrition link practitioners in each locality, who updated the folder and shared the information.
The training programme covered why to screen for malnutrition, when to screen and how to screen using the community MUST. It also included how to estimate BMI using the mid-upper arm circumference (MUAC) and how to estimate height using ulnar length. Attendees were given opportunities to practice, and case studies were used to assist in confidence building. The programme also covered the delivery of good, initial food-first advice and the resources available to support this.
Lastly, the training sessions were supported by the annual update on enteral feeding presented by the homecare nurses from Abbott. This annual update is a mandatory requirement in the trust, and to promote attendance, the nutrition nurse specialist and the nutritional lead nurse developed a whole day's teaching programme, which was offered 4-6 times over the year. The day included an update on management of enteral feeding tubes, MUST screening, end-of-life feeding dilemmas and case studies, and the feedback for these has been overwhelmingly positive.
Referrals
To ensure that patients are seen and managed appropriately, the community nutrition nurse specialist developed a referral form, which aimed to ensure that any patient identified with a MUST score of 2+ was referred to the nutrition nurse. The rationale for this was twofold: (1) to ensure that patients were managed on the correct pathway and (2) to try and identify the scale of the problem across the district nursing caseloads in Buckinghamshire. It was also hoped that, by referring in the first instance to the community nutrition nurse specialist, there would be a reduction in inappropriate referrals to community dietitians.
The community nutrition nurse specialist maintains a database of all referrals. Some 43 patients were referred from June 2018 to 31 December 2018. Not all referrals required a visit: some required information, which was provided by the district nurse, and three patients died before a visit could be arranged. From January 2019 up until the end of July 2019, 54 patients were referred to the community nutrition nurse specialist. Three patients declined a visit, four were referred on to dietitians, and the rest were sent information. The community nutrition nurse specialist holds a caseload and documents using RIO. A number of patients have been discharged following a period of monitoring and support.
To support families and carers, the community nutrition nurse specialist develops management plans, which include meal advice, shopping lists and ways to enrich and fortify diets. Visits with patients generally last between 45 and 90 minutes, during which time, the patient is weighed and received MUST screening. All patients are given specific information tailored to their circumstances. If, after two visits, there is evidence that the advice has not been taken on board, patients are not making progress or are continuing to lose weight unintentionally, a referral is made to the community dietetics team for more specialist advice.
Any referral made to the community nutrition nurse specialist for which a more serious concern is identified automatically referred to the community dietitian team. These would be, for instance, patients with complex medical conditions, such as organ failure, and those whose nutrient levels and dietary needs required management by a dietitian.
Alongside the referrals and teaching, the community nutrition nurse specialist reviews complex feeding requests for the district nursing team, for example, for patients who may require enteral feeding by bolus doses multiple times a day and those who have no support at home. This is to ensure that, when a patient is being discharge with complex feeding requirements, there is capacity within the team to accept the patient in the short term as well as an ongoing robust management plan. Following a number of complex referrals and lack of social care support, a guidance document has been produced by the clinical lead nurse and the community nutrition nurse specialist outlining what capacity the district nursing caseload might have and what is not achievable.
Outcomes
Since the introduction of the community nutrition nurse specialist role, all patients are being screened effectively with a validated tool, and districts nurses are providing nutrition advice with more confidence, which is helping patients be more proactive in their food choices and how they manage their malnutrition risk. While there has been general improvement in knowledge and confidence among the district nursing teams, this has not been universal. An ongoing programme of education and support is now in place. The nutrition-related advice provided now is more personalised, as the nurse specialist can spend quality time with patients and provide tailored food plans and shopping lists. Further, the nutrition risk for a number of patients has been reduced, which has meant that dietitians have not needed to be involved.
At present, an audit of the community MUST and compliance for pathway use is being undertaken. Further, the knowledge questionnaire has been re-administered, and the results are being analysed.
Conclusion
The role of the community nutrition nurse specialist in Buckinghamshire is a new and innovative one, which continues to evolve. Its focus is to ensure that patients who are identified as being at risk of malnourishment by the district nursing and community adult teams are quickly assigned to the appropriate pathways and the effectiveness of the process is monitored. Malnutrition has a significant impact on both quality of life for patients and costs for the health service. Therefore, its early detection and management are vital, and it is hoped that the introduction of innovative roles such this one will help improvement the management of malnutrition in the community.

