In healthcare, medicines are the most common forms of intervention, helping to prevent, treat and manage many conditions or illnesses (National Institute for Health and Care Excellence (NICE), 2015). The rise in multimorbidity and polypharmacy, along with new models of delivering acute care, means that support services must be strengthened to ensure the safe and effective use of medicines in the community. Between 5 to 10% of all hospital admissions are medicines-related (Kongkaew et al, 2008; NICE, 2015), of which, two-thirds are potentially preventable (Howard et al, 2007).
NICE define medicines support as any support that enables a person to manage their medicines (NICE, 2017). In practical terms, this would include general support, such as reminding or prompting a person to take their medicine or supporting them with administration of medicines.
As the law stands, a person administering a prescription-only medication (POM) to anyone other than themselves must only do so under the directions or instructions of a prescriber (The Human Medicines Regulations (HMR), 2012). It is the responsibility of the organisation to define within their policies who can administer medicines, but those given or delegated this responsibility must be appropriately trained and assessed as competent (Royal Pharmaceutical Society/Royal College of Nursing (RPS/RCN), 2019).
Individuals in the community are often aided by social care practitioners to take their medicines, with community nurses usually administering complex medicines that require invasive or more specialised administration techniques.
When health or social care practitioners administer medicines, there must be a clear, accurate and immediate record of all medicines that are administered, withheld or declined (RPS/RCN, 2019). This is usually in the form of a medicines administration record (MAR) chart. MAR charts and their use enables auditable, safe and effective practice in the community when supported by clear policies. Many social care providers receive their MAR charts from a community pharmacy, whereas community nurses have traditionally relied upon general practitioners (GPs) to complete MAR charts. A MAR chart does not provide instructions on medicine administration; rather, the chart keeps record of the medicines that have been administered.
Some GPs may be reluctant to provide a written MAR chart, as a prescription is all that is legally required for a third party (for example, a nurse or care worker) to administer medicines (British Medical Association, 2018). GPs are under no obligation to provide any charts under the NHS contract for general medical services (GMS). This can present some difficulties as nurses need to adhere to their local policies, yet prescribers are within their rights to refuse to complete a chart.
Nurses who are not qualified prescribers can only administer POMs through a signed prescription, a signed patient specific direction (PSD) or a patient group direction (PGD). A primary care prescription form (for example, FP10, WP10, GP10, HS21–depending on the country), can act as the authority for a pharmacist to dispense the medicines and for a third party to administer them. However, the prescriber has a duty of care to ensure that written prescriptions should include clear instructions on how the medications should be safely taken. These should also provide a clear dose and directions for administration.
The term ‘as directed’ or equivalent would not constitute a clear enough instruction for a third party to follow, unless this is supplemented by other forms of instruction (such as verbal) from the prescriber to each individual health or social care practitioner responsible for administration. Thus, if the employer of the community nurse (or other practitioner) requires a MAR chart, the responsibility for completing it resides with the organisation whose employees are using it, compiled from the information provided by the prescriber and completed by staff trained in the process.
Understanding current practice
In Wales, district nursing teams have highlighted concerns about accessing MAR charts in a timely way and are actively seeking solutions, which includes transcribing of medicines. Transcribing is defined as making an exact copy of previously prescribed medicines to enable their administration in accordance with the instructions of a prescriber (NICE, 2015). Transcribing can be carried out by any registered nurse using a variety of sources, such as previous MARs, medicine labels or discharge summaries. A prescribing qualification is not required to undertake transcribing, but the nurse must be appropriately trained, assessed as competent to do so and should be working in line with their local transcribing policies and procedures (RPS/RCN, 2019).
These concerns were discussed at the All Wales District Nursing Forum (AWDN), a group which represents district nursing and provides professional advice in Wales, along with clinical pharmacy and digital medical leads. The view of the forum was that access to MARs was an issue across Wales, with some DN teams experiencing more difficulties than others. The Forum also expressed concerns as transcribing is an unfamiliar practice for district nurses (DNs). One of the other possible issues included how nurses would be able to confirm current medications (for example, through GP records and the risk of making errors when transcribing medicines).
As a result of this, an anonymised electronic survey (Table 1) was designed by the authors and set up by the Strategic Programme for Primary Care (2022), to understand the views of nurses working in district nursing teams across Wales. The survey was carried out on two separate occasions, in September 2021 and in April 2022. This was because after the first survey, a task and finish group set up by the AWDN Forum requested a repeat survey to try and increase participation across all health boards.
Table 1. Electornic Survey to understand the views and concerns on access of nurses working in district nursing teams in Wales regarding access to medicines administration record charts
| Question no. | Questions | Options |
|---|---|---|
| 1 | Which Health Board area do you work within? | Aneurin Bevan University Health Board Betsi Cadwaladr University Health Board Cardiff and Vale University Health Board Cwm Taf Morgannwg University Health Board Hywel Dda University Health Board Powys Teaching Health Board Swansea Bay University Health Board |
| 2 | Do you use a drug chart to record the administration of medication? | Yes No |
| 3 | What are the most common drugs administered by district nurses (tick all that apply) | Insulin Warfarin Low molecular weight Heparin B12 End-of-life care drugs Gonadotrophin-releasing hormone analogues (GnRHa) eg Prostap and Zoladex Other (please specify): |
| 4 | Is there difficulty accessing or getting updated drug charts from GPs? | Yes No (please explain current arrangements in place to access drug charts) |
| 5 | Are there any difficulties accessing drug charts for the following: | Insulin Warfarin Low molecular weight Heparin B12 End of life care drugs Gonadotrophin-releasing hormone analogues (GnRHa) eg Prostap and Zoladex Other (please specify): |
| 6 | Which of the following drug charts do you use? | Insulin General medication, eg. B12 End of life medication Other (please specify): |
| 7 | Do difficulties in accessing or getting updated drug charts increase out of hours? that is, between 6 pm–8 am and/or at weekends? | Yes - accessing new drug charts Yes - accessing changes to drug charts No General comments: |
| 8 | Can community/district nurses currently access general practitioner (GP) records? | Yes No |
| 9 | What benefits would you see in having access to GP records? | Comments: |
| 10 | What are your thoughts about transcribing medication? (tick all that apply) | Yes - if this was supported by clear policy, guidelines and training Yes - for some medication if this was supported by clear policy, guidelines and training Yes - I feel this would save time No - I do not feel this is a nurse's role No - this is a GP's role No - I would have concerns (please specify) |
| 11 | Please share any other comments you have | Comments: |
Key Findings
A total of 286 responses were received from both surveys, with an additional 10% of the responses received in the second. All seven Health Boards took part, although participation varied from 5% to 31%. However, it was noted that some respondents replied on behalf of the whole team, rather than each team member completing the survey individually.
Types of medicines administered by district nursing teams
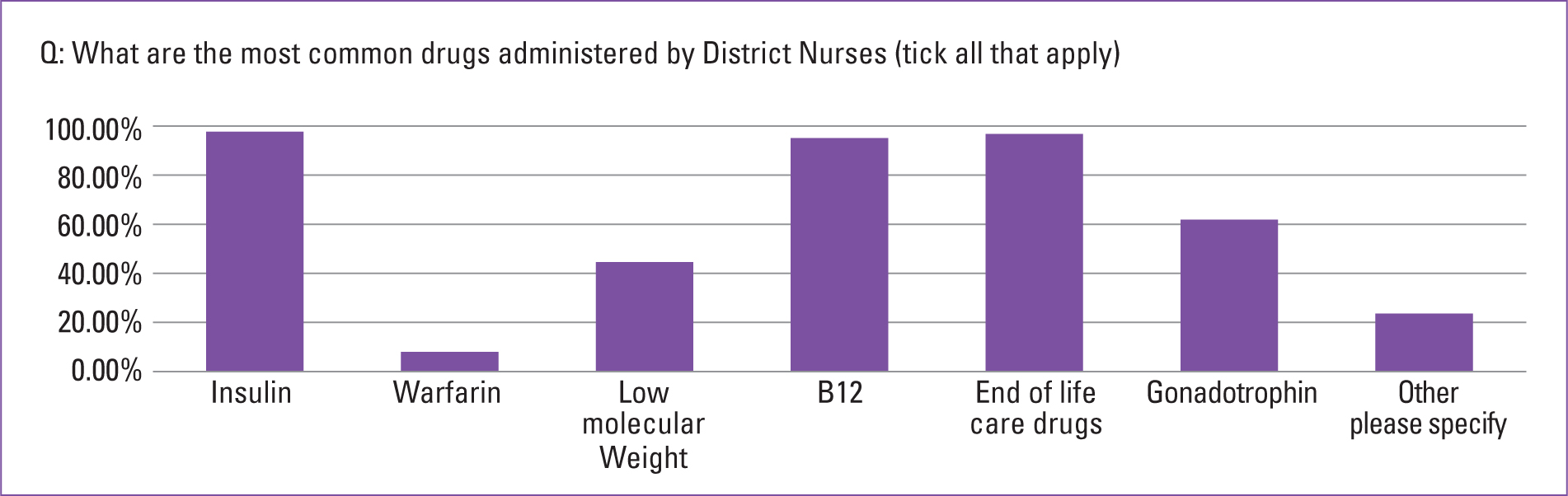
The most common medicine administered by 98% of survey responders was insulin, followed by medicines used for symptoms management at the end of life (96%) and hydroxycobalamin (95%) (Figure 1). Two other categories of frequently administered medicines were gonadotrophin releasing hormone analogues, such as Prostrap, Zoladex (62%) and low molecular weight heparin (45%). Other medicines included intravenous antibiotics, medicines for bowel or catheter management and treatments related to the management of cancers.
Types of medicine charts used
While the majority of nurses used MARs to record the administration of medicine, 6% did not. However, discussion at the AWDN forum indicated that where MAR charts were not used, medicines were recorded in the person's clinical record.
A variety of MAR charts were in use. Apart from charts use for general administration, additional charts were used for insulin (by 98% of respondents) and end-of-life charts (96%).
Issues concerning access to MARs
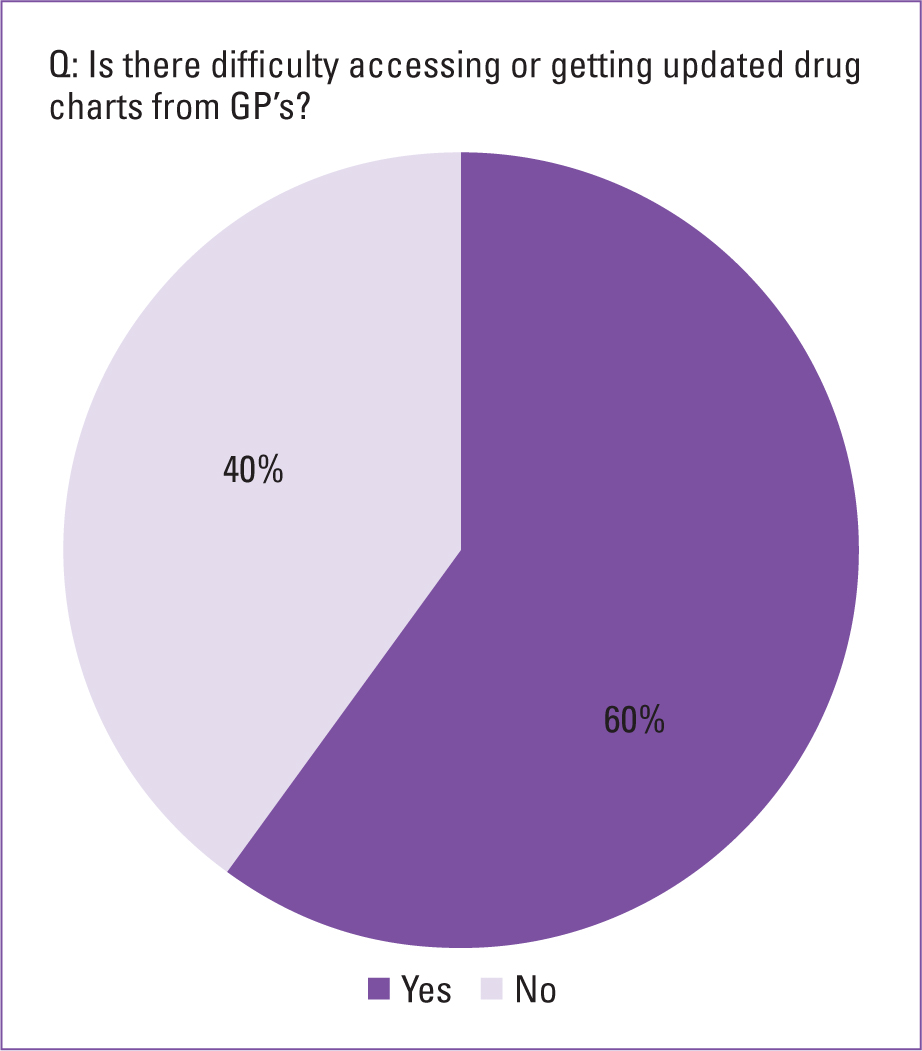
A total of 60% of nurses experienced difficulties in accessing MAR charts (Figure 2). A particularly problematic time for accessing MARs charts was perceived to be between 6pm-8am and over the weekends. This applied to out of hours requests for both, medicine changes to existing MARs and requests for new MARs.
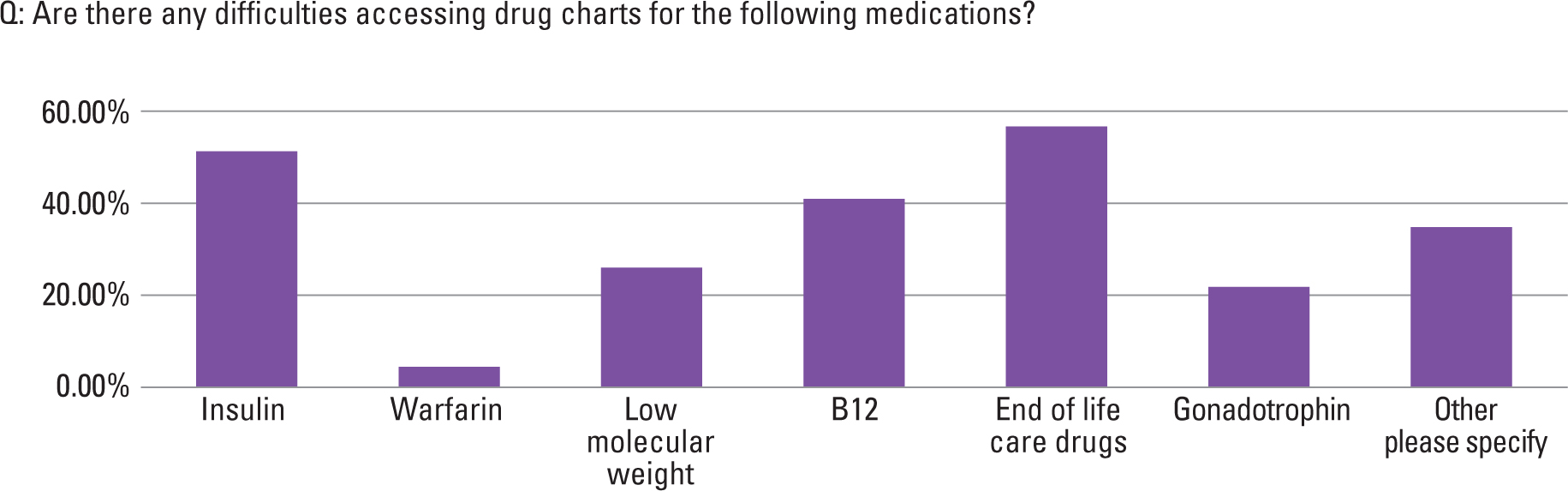
Accessing MARs for end-of-life medicines, insulin and hydroxocobalamin were most frequently mentioned (Figure 3). An analysis of comments indicated that most often nurses collected MARs from the GP practice. Other ways used to access MARs included email or during multi-disciplinary meetings. However, it was clear that where nurses were required to pick up MARs, this had an impact on nurses' time, through additional travel to and from the GP practice and in waiting for GPs to complete the charts. Nurses reflected on how this impacted the care they provided, especially for those at the end of their life. In some instances, the impact was noted to be more on family or relatives, who would have to travel to collect MARs. While asking family or relatives to pick up MARs is a sensible approach, it may not be possible for some.
Difficulties in obtaining MARs following a person's discharge from hospital were also mentioned. Examples included delays in the completion of MARs, MARs not sent home with the person and a reluctance to prescribe medicines started by a consultant. Some nurses also noted how MARs could be inaccurate or not signed, resulting in further delays. This perception by nurses that charts must be signed, suggests that nurses view MARs as a legal requirement for them to administer from, rather than an organisational one.
Access to medical records by DN teams
The survey found that 31% of nurses had access to a clinical record (Figure 4). However, these records still seemed to have access restrictions. For example, only DN team leader's had access; access was available only during the practice's opening hours or was limited to certain practices within clusters. This meant that during out of hours periods, there could have been further limitations on accessing GP medical records.
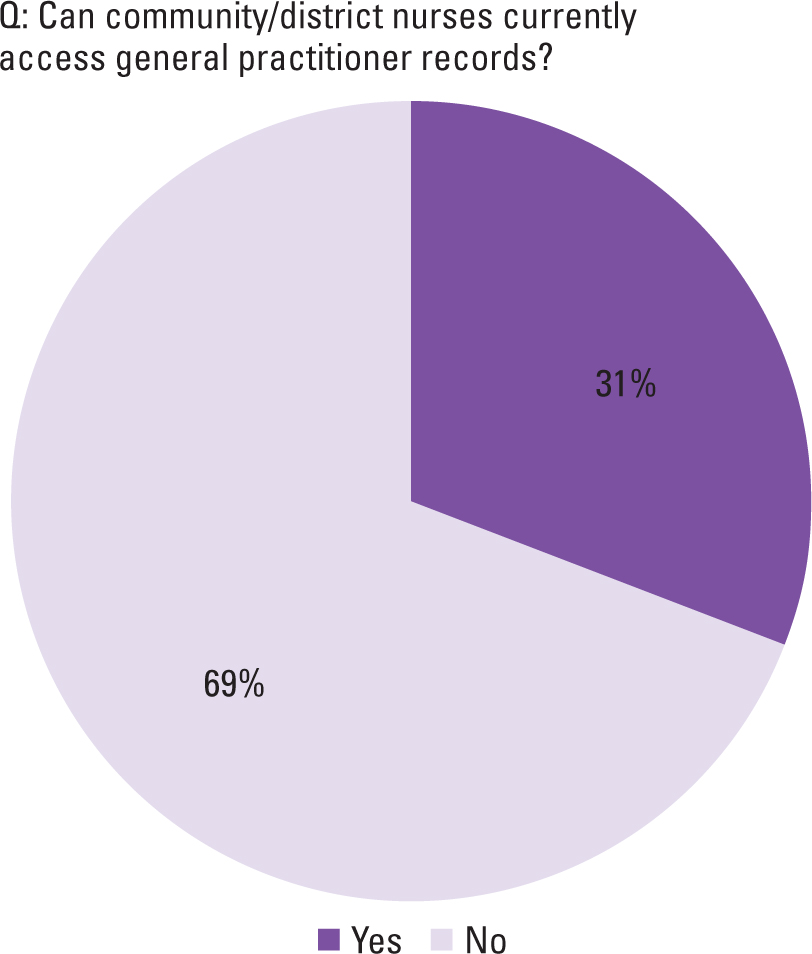
However, where nurses were able to access the person's medical records, the benefits were clear. Common reasons mentioned by nurses for such a positive perception included: being able to see up-to-date and accurate information, current medicines, allergies, past medical history and recent consultations. It was also clear that nurses felt such access to medical records would benefit the person in terms of providing better, seamless care, improving continuity and saving both the nurse's and the GP's time.
Nurse's views on transcribing
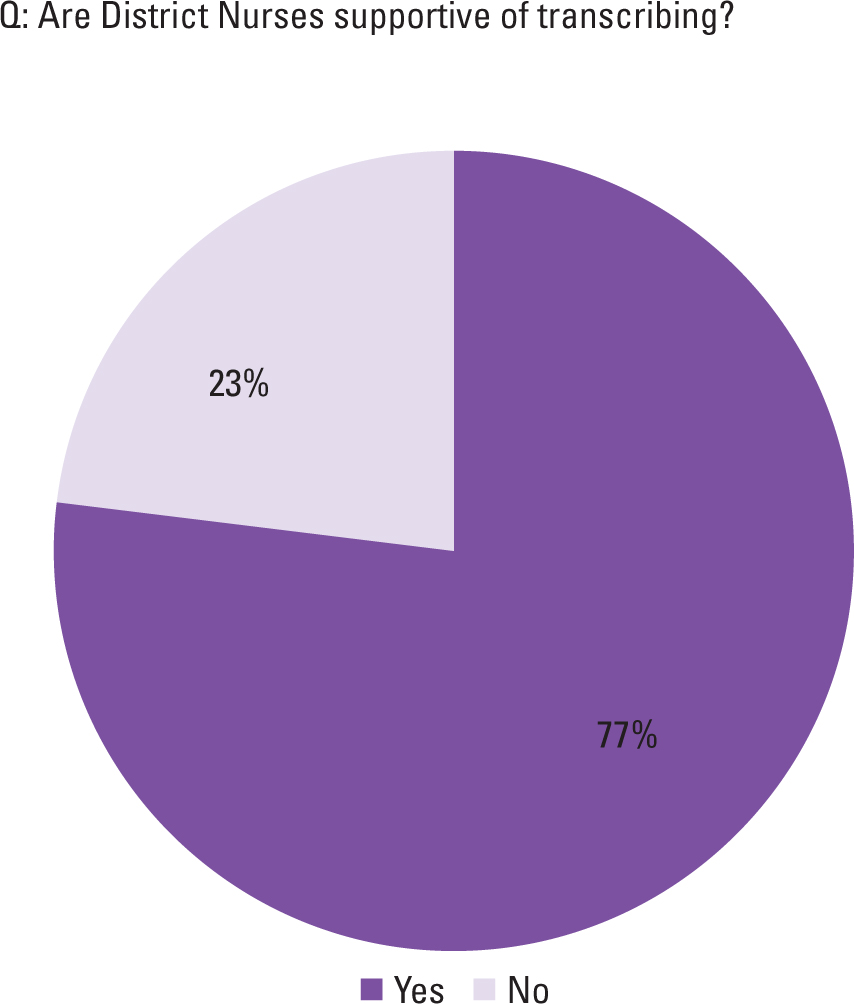
Nurses were given the option to choose several responses in order to better understand their views and concerns regarding transcribing. Overall, 77% of respondents agreed with the use of transcribing (Figure 5), if supported by either clear policies, guidelines and training (25%) or if used for some medicines only (31%) (Figure 6).
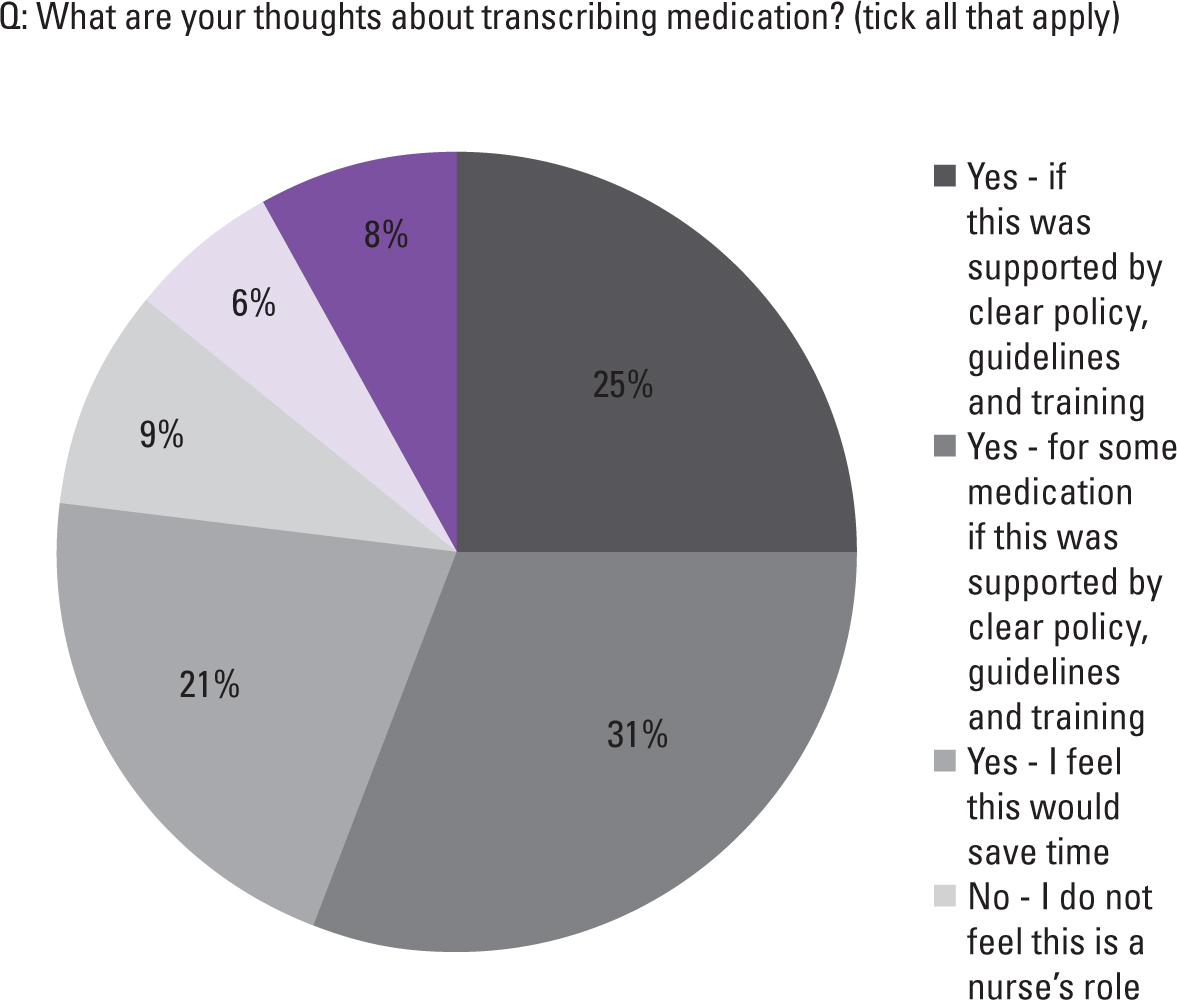
In general, it was mentioned that transcribing was suitable for medicines such as insulin and hydroxocobalamin, but less so for controlled drugs. Some said they did not see transcribing as a nurse's role (9%), or they would not use it as they would have concerns (8%). Another 6% of nurses said transcribing should only be the GPs' role. While some of the comments recognised how transcribing could save time and support people's care, others raised concerns. These included:
- Risk of errors; for example, where changes to medicines had not been communicated, or for junior colleagues who may be less knowledgeable regarding the medicine being transcribed
- Additional work for nurses already under significant pressures, which may negatively impact on people's care
- Lack of timely access to information regarding current medications.
Discussion and implications for practice
This survey was undertaken to understand current working practices in district nursing teams regarding access to MAR charts and nurses' thoughts on transcribing. Despite initial concerns about transcribing from the AWDN forum, most nurses thought it would support their practice. Nurses had conflicting opinions on whether they should be able to transcribe any medicine, or only specific ones.
The Code (Nursing and Midwifery Council, 2018) contains professional standards for registered nurses and nurse associates, and has four themes. Of particular relevance to the findings of this survey, are ‘practice effectively’ and ‘preserve safety’. For example, the survey identified delays in nurses accessing MAR charts, which may prevent people accessing medicines in a timely way. The use of transcribing could help promote the person's best interests, preventing delays and unnecessary harm or distress (HMR, 2012). While nurses had differing views on the types of medicines that could be transcribed, the Code (NMC, 2018) is clear about nurses seeking help for any ‘action or procedure that is beyond the limits of your competence’. Transcribing is a process, which, if supported by clear policies and training, should result in nurses feeling confident regardless of the medicine being transcribed. This suggests that any medicine could be transcribed, as long as the nurse feels competent.
However, guidance notes that care should be taken for certain high-risk medicines (RPS/RCN, 2019). These include medicines that are commonly administered by the DN service such as insulin, anticoagulants and controlled drugs. While nurses were not asked to specify which end-of-life medicines were requested, nurses may also have concerns about transcribing other medicines commonly used, such as anxiolytics, benzodiazepines or antiemetics. This is an area which needs further discussion by the all-Wales sub-group and its possible inclusion in future policies.
There have been misconceptions that a MAR chart must be completed by someone with a prescribing qualification; however, this is not a prescribing activity. Information regarding transcribing is included within the ‘professional guidance on the administration of medicines in healthcare settings’ document (RPS/RCN, 2019). Charts used in hospitals often have a dual purpose, providing patient-specific directions and include sections to allow recording of medicines administration. In the community, medicines have usually already been prescribed; therefore, the purpose of the chart is to record administration, and thus, does not usually require any involvement of a prescriber.
To implement transcribing, nurses require information about the person's current medicines, including frequency of administration and any special instructions (for example, ‘take with food’). On dispensing, the pharmacy is required by law to transfer the relevant information from the prescription on to the medicine packaging as per HMR (2012). The dispensing label, provides the nurse with the authority to administer, as this reflects the prescriber's intentions. However, some prescriptions, and thus pharmacy labels, do not contain sufficient instructions to support nurse transcribing, such as when GPs write ‘to be used as directed’ on the prescription, or if changes to insulin doses are recommended by a diabetic specialist nurse. Therefore, there are implications for how changes to medicines are communicated to GPs from other practitioners, alongside support to GPs to both understand what information nurses require to safely transcribe, as well as how transcribing can support nurses, the patient and themselves. This will be in addition to the training nurses will require to transcribe safely as recommended by guidance (RPS/RCN, 2019). Finally, transcribing will need to be underpinned by clear policy and guidelines for nurses—an area of practice being currently developed by the sub-group.
Nurses perceived GPs as not always knowing how to correctly complete MAR charts, which was often cited as causing delays. Currently, there is no all-Wales standard MAR for community services, which is a recommendation in the All Wales Medicines Strategy Group (AWMSG) 5-year strategy (2018-2023) (All Wales Medicines Strategy Group, 2018). The results of this survey and a desire to support the development of transcribing, offers an opportunity to create a standardised MAR, designed to support easier completion by GPs and nurses when transcribing. This may help prevent errors when transcribing, a common area of concern for nurses taking part in the survey. Additionally, a standard MAR means nurses working across services will be familiar with the chart, which may also help prevent administration errors from occurring.
The survey found that not all nurses had access to GP medical records. While this does not prevent nurses from transcribing, it does provide nurses with the ability to confirm current medicines and allergies and see recent consultations and documentation, such as discharge letters. These are clinical safety aspects which are important to the quality of care provided to an individual and strengthen clinical governance processes. Indeed, it could be argued that a lack of access to clinical records undermines nurse's professional decision-making, particularly where a person's condition is rapidly changing. This is particularly true in cases such as when dealing with patients at the end of life or where quick intervention could prevent an unnecessary admission to hospital. With an increasing focus on supporting individuals at home and a 2-hour response period (NHS England, 2021), it is evident that systems which support nurse's professional decision-making is required. Therefore, further work is essential to understand how nurses can be supported to access people's medical information in a timely manner.
Lastly, this work appears to have identified an area of practice where there is limited recent research on transcribing in district nursing services and the views of nurses who have been asked to undertake this. This may be because of the rise in independent prescribers within district nursing teams, or the existence of different processes in place to support nurses' access to MAR charts.
Conclusion
Medicines support is a key area of practice familiar to nurses working within district nursing services. Concerns resulted in a survey to understand how access to MAR charts could be improved and to identify possible solutions. This study provided an opportunity to understand the types of medicines administered and nurses' views on transcribing—an area of practice which is not often reflected upon.
This study found that 60% of nurses experienced difficulties in accessing MAR charts, particularly during out of hours periods. Overall, 77% of nurses supported transcribing as a possible solution.
There needs to be clear policies and training in place, supported by nurses having access to the person's medical records and introducing a standard MAR chart. This would enable nurses to have greater confidence in transcribing medicines, promoting safe and timely administration to people seen by the district nursing service.


