References
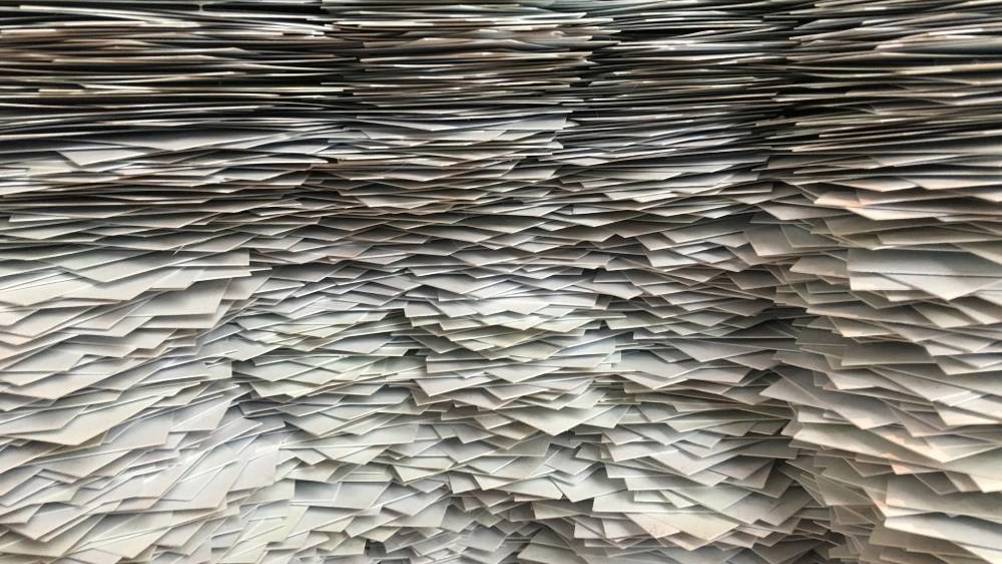
Paperlite: piloting a new way of working in community nursing
Abstract
Technology within healthcare is a growing industry, and health professionals now use technology within their everyday working life. Within hospitals, it is the norm to see staff using handheld devices to record clinical observations and patient notes being typed into an electronic system. However, the use of technology within community settings is far behind that of hospital counterparts. It has been acknowledged that the use of technology in healthcare will improve efficiency and remove some of the bureaucracy within the NHS, and community areas are beginning to pilot different ways of implementing this. This article describes a pilot trial of using technology to aid mobile working in the author's trust and discusses how district nursing can embrace the use of paperlite culture to improve efficiency and record reliability.
Society at large has become reliant on technology in a relatively short space of time, and the timescale in which technology has progressed is impressive. Consider the moon landing, which was 50 years ago; today's smartphones have far greater computing ability than the computer that aided the moon landing mission (Kaku, 2011). We now live in a world where good technology is essential for good communication, creating and maintaining a community (through social media) and working efficiently, and the world of healthcare is catching up. Certain countries have been pioneers in the adoption of health technology, and have used it for many years. Denmark has been ahead of the trend for some time, introducing basic electronic prescriptions in the 1990s, and Sweden quickly followed its lead (Klein, 2010). In Denmark, clinicians across all regions are able to access a patient's health records (Danish Ministry of Health et al, 2018). In terms of telehealth, India is developing this area for its many rural areas that do not have regular access to doctors (Rao, 2018).
Register now to continue reading
Thank you for visiting Community Nursing and reading some of our peer-reviewed resources for district and community nurses. To read more, please register today. You’ll enjoy the following great benefits:
What's included
-
Limited access to clinical or professional articles
-
New content and clinical newsletter updates each month

