Intermittent self–catheterisation (ISC), also frequently known as clean intermittent self-catheterisation, is the procedure of artificially emptying a dysfunctional bladder. Identified and developed by Jack Lapides over 50 years ago (Lapides et al, 1972; Angermund et al, 2021), the procedure involves passing a hollow tube (or catheter) into the bladder to drain off urine when clinically indicated, with the catheter then being immediately removed (Doughty and Lister, 2015). ISC may be used for short-term use, such as voiding problems after surgery (e.g after botox injections into the bladder or post–partum voiding difficulties) or may be a long-term management solution for individuals with bladder dysfunction (e.g. multiple sclerosis (MS), spinal injuries). It has long been identified as the ‘gold standard’ compared to urethral or supra-pubic indwelling catheters (National Institute for Health and Care Excellence (NICE), 2015). This is because it allows independent periodic filling and emptying of the bladder, with a specially designed nelaton (in/out) catheter (Figure 1), which does not have a retaining balloon. Thus, it mimicks normal bladder filling and emptying. This technique has shown to reduce urinary tract infections (UTIs) (Yates, 2013; 2017), promote a ‘normal’ pattern of micturition, and can improve independence and quality of life (Leaver, 2022).

Prevalence of the use of ISC is scant; however, statistics show that approximately 50 000 individuals in the UK use ISC (Wilks et al, 2020). Approximately 1 in 10 men over the age of 70 years, and almost 1 in 3 men in their 80s will develop acute urinary retention (Bladder Interest Group, 2021), which may require ISC. The MS Society has reported that 9 in 10 people with MS will have a bladder problem at some point, while 80% of those who have experienced a spinal cord injury will have some degree of bladder dysfunction. All of these identified individuals may require ISC at some time to maintain bladder function. It is difficult to obtain costs for community use compared to acute settings, but it is indicated that 1.5 million prescriptions were issued in England in 2021 at a cost of £145.8 million (Bladder Interest Group, 2021) with regards to catheter use and care. However, they do not make the distinction between indwelling urinary catheters and ISC.
Indications for use of intermittent self-catheterisation
The indications to undertake ISC are numerous (Box 1); however, not all individuals will be suitable or capable of undertaking the procedure. Children aged as young as 4–5 years can be taught the technique, as can older people if they are accounted for their specific needs. Thus, suitability for ISC depends on individual assessment, presenting symptoms and individual training needs. Assessment should include the presenting symptoms such as frequency of urination, urgency, nocturia (getting up at night), hesitancy or symptoms of stop/start flow, any urinary leakage, and should also include bowel patterns and medication, as well as previous medical history. Vital investigations include bladder diary and fluid intake, and pre- and post-void residual urine scan to ascertain total bladder capacity (compared to residual volume and urinalysis).
Box 1.Indications to undertake intermittent self-catheterisation (ISC)
| Rational for undertaking ISC | Common causes to undertake ISC |
|---|---|
| Failure of bladder outlet to open to allow passage of urine (e.g. enlarged prostate or surgery for stress urinary incontinence) | Enlarged prostate, or surgery for stress urinary incontinence |
| Detrusor hypocontractility/reduced or absent bladder contractions | When the muscles of the bladder wall (detrusor muscle) fail to contract to expel urine (e.g. neuropathic conditions such as multiple sclerosis, spinal injuries, cauda equine, spina bifida, diabetes, cerebro-vascular accident, some forms of Parkinson's disease or medicines) |
| Procedures/medication/instilled drugs that affects the contractility of the bladder muscle (detrusor muscle) | Botox, chemotherapy |
| Management of urethral strictures. To prevent reoccurrence of stricture and maintain patency of urethral orifice | Infection such as chlamydia; trauma, including surgery to urethra (urethrotomy) |
| Obstruction causing difficulty in emptying | Constipation; prolapse; pregnancy |
Adapted from: Rantell (2012); Yates (2013, 2017); Royal College of Nursing (2021)
All training should be undertaken by a competent health care professional (Royal College of Nursing (RCN), 2021) and at the individual's own pace. This may indicate that they may require more than one session.
Healthcare professionals should also consider if the individual:
- Is able to store urine in their bladder
- Has an understanding of the anatomy/physiology of the lower urinary tract
- Has the ability to visualise urethral meatus
- Has a reasonable level of cognition to be able to comprehend rational for ISC instruction and capacity to follow verbal/non-verbal instructions
- Has a good level of dexterity to hold the catheter and has enough mobility to position themselves correctly
- Is motivated and committed to the use of ISC as it may potentially be long term
- Has sufficient bladder capacity to remain continent between catheterisations
- Will be aware of how to avoid potential problems associated with ISC
- Will be able to recognise when a potential problem exists
- Will be able to contact appropriate healthcare professional, when required
- Is advised how to reorder and store catheters correctly (RCN, 2021).
However, there are also a few contraindications to ISC. These include individuals with a false urethral passage, trauma to the urethral area, high intravesical pressures in the bladder which require free drainage to avoid renal damage or where accurate urine monitoring is required (Leaver, 2022).
It is also important to note that while ISC has numerous advantages, it also has some limitations (Box 2).
Box 2.Advantages and limitations of intermittent self-catheterisation (ISC)
| Advantages | Limitations |
|---|---|
| Maintains normal bladder function and protects upper tract from ‘reflux’ | Physical disabilities, poor eyesight, reduced manual dexterity, reduced mobility, urogenital prolapse or large abdominal apron |
| Reduces urethral trauma and fewer urinary tract infections than associated with indwelling catheters and reduces catheter-associated problems (e.g. blockage due to encrustation, erosion) | Psychological barriers to using the technique (e.g. fear of pain, anxiety of perceived discomfort, concern about sexual function) |
| Less risk of urinary leakage and incontinence | Poor understanding of anatomy of urinary tract and rational for ISC |
| ISC is discreet to use and reduces the need for other appliances/pads to manage continence | Small total bladder capacity (under 200 mls) as this would require frequent ISC |
| No need for drainage bags associated with indwelling catheters, which allows greater choice in clothing | Religious/cultural beliefs |
| Improves independence and body image, and allows increased ability to join in leisure activities | Time-consuming, especially outside of home (e.g. finding a clean public toilet) |
| Improves quality of life, increases self-confidence, improves sleep, ability to remain sexually active, promotes dignity | Technical difficulties associated with slippery catheters |
Adapted from: Doughty and Lister (2015); Yates (2013; 2017); Logan (2018)
Catheter selection
A wide range of intermittent catheters are available on the drug tariff and it is imperative that the healthcare professional understands the benefits and disadvantages of each. This would give the patient the most optimal chance of succeeding and maintaining the procedure. All intermittent catheters require lubrication prior to insertion and this can be done in a number of ways. Some come pre-lubricated, while others come with their own water/gel supply. There are also some intermittent catheters that require a separate lubricant.
Intermittent self-catheters can include the following:
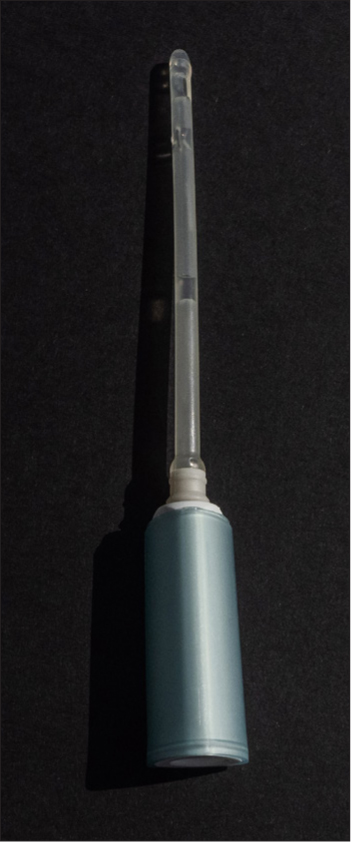
- Hydrophilic-coated (single-use): these require water to activate and hydrate the coating and some come with their own water supply (Figure 1)
- Pre-gelled (single use): these have gel in the pack
- Reusable nelaton catheters (single patient use): these can be used with water-soluble lubricating/anaesthetic gel. This type of catheter can be reused at home as it can be cleaned with soap and water/boiled/disinfected/microwaved, air dried and stored in a plastic bag/box according to the manufacturer's instructions. In vitro studies have indicated that cleaning of the catheter was more effective if a solution of diluted milton was used (Wilks et al, 2020). However, it is worth noting that these catheters are rarely used in the UK.
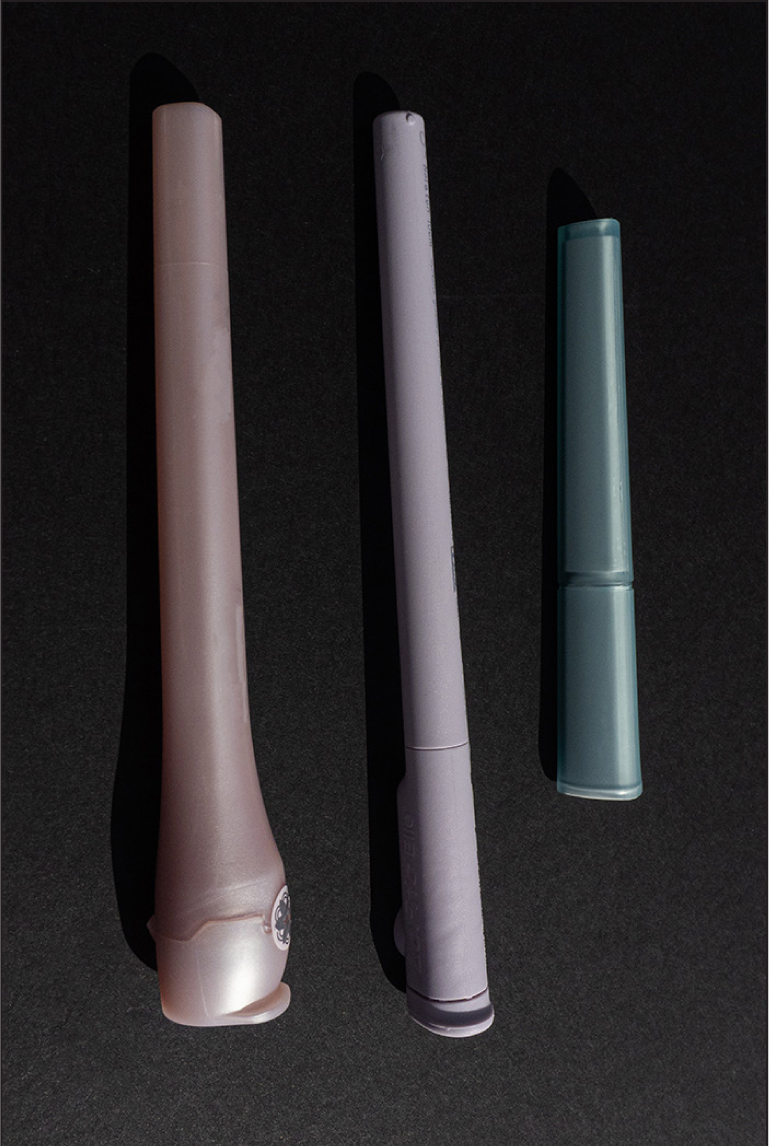
The type of catheter used should be guided by research and patient choice (RCN, 2021). The Charrière (Ch) or French gauge is the external diameter of the catheter. Sizes range from 6–24Ch. Normally, 10–14Ch would be used for adults, while 16Ch or higher would be used for dilatation. Intermittent self-catheters also come in different lengths; a standard catheter would range from 40–45 cms; while catheters for females are usually 25 cms (Figure 2) (Leaver, 2022). Some manufacturers produce compact and telescopic catheters which extend to produce the correct length (Figures 2 and 3). Some manufacturers now produce infection control intermittent self-catheters with or without the intergral bag attached (Figure 4). Intermittent self-catheters with integral bags can be beneficial when the individual is not in the vicinity of a toilet, if they are wheelchair-bound or cannot get onto a toilet for any reason (Leaver, 2022).

Instruction for use
Instruction of ISC requires excellent communication skills on behalf of the healthcare professional. The rationale for the intervention needs to be conveyed appropriately to the individual. Individuals informed of the need to do ISC usually feel anxiety, shock, embarrassment, apprehension and fear. They need to be well-informed as to why they have to undertake the procedure, how it will impact their lives (and family life), if it will cause internal damage, how often they will need to do it, what risks are associated with the procedure and if it will be for life. Furthermore, they should be assessed for any aids, devices or equipment required to make ISC easier (e.g. if they have poor dexterity, hand grips should be installed; leg separators, mounted mirrors to make visualisation of urethra easier, are all available for assistance). The professional should inform them that the main outcomes of initiating ISC is to improve their quality of life and to protect their kidney function, but that there are also other benefits associated with procedure (Box 2). This instruction should be supported by the use of DVD videos and written information, and may require more than one session with the individual and should be undertaken at their pace (Yates, 2017). The individual should be instructed until they feel confident and comfortable to undertake ISC safely unsupervised (Box 3).
Box 3.Procedure for teaching intermittent self-catheterisation (ISC)
| Action | Rationale |
|---|---|
| Prepare the individual for ISC with documentation/videos/information | To understand the rational for introducing ISC |
| Gain individual's informed consent and check knowledge of ISC | |
| Check individuals capability and motivation of performing ISC | Are any special devices/aids/equipment needed. Try to motive by giving information |
| Assemble equipment required range of intermittent self-catheters | So individual has a range to choose from what suits them |
| Individual should choose most appropriate place and position | E.g. Bed, bathroom, over the toilet. They may want to sit on toilet, stand over toilet, one leg elevated on stool, sit in wheelchair or on bed. This may also influence catheter selection |
| Teach importance of hand hygiene, including nails | Prevent complications of ISC and infections |
| Prepare catheter according to manufacturer's instructions | To make sure of correct insertion and prevent complications |
| Advise individual to try to pass urine | Only what is left is true residual and this is what the frequency will be based on |
| Advise to wash genital area. Females from front to back towards anus. Males should retract foreskin to clean glans | Prevent cross contamination and infection |
| Females should part labia with non-dominant hand to identify urethra (some use a mirror). Men should hold penis in non-dominant hand in an upward direction towards stomach | To correctly identify route for catheter entry. This helps to extend urethra and makes it easier to insert catheter |
| Gently insert catheter with dominant hand while pointing funnel into toilet or collection receptacle. Avoid touching part of the catheter that will enter urethra | Correct drainage technique and prevents infections |
| Continue to insert catheter until urine flows | To empty bladder |
| When urine stops, individual should gently remove catheter, slowly rotating to allow full drainage of bladder | Allows full drainage of bladder on the removal of catheter |
| To avoid dribbles or spillage, place a finger over the funnel to trap any urine before finally removing | Prevents spillage |
| Dispose of catheter as per manufacturer's instructions | Do not flush down toilet; dispose off correctly |
| Hand hygiene | Prevent contamination |
| Check individual is at ease with procedure and happy to continue unsupervised | Promotes independence for ISC but also identifies if further assistance required |
| Provide information leaflets of fluid intake, bladder diary, signs of infection, catheter supplies, contact details | To evaluate the benefits of the ISC, maintenance of skills and review of frequency. Order future supplies or contact if advice is required or if complications arise |
| Document in records procedure, catheters used and supplies | To provide a point of reference or comparison for future queries |
| Follow up | To review all of the above |
Adapted from: Vahr et al (2013); Doughty and Lister (2015); Yates (2017))
They should be informed and instructed on a no-touch technique in order to avoid contamination of the catheter and the frequency of ISC required. They should also be advised on the different catheter types; they may want to use different catheter types for different activities throughout the day such as infection prevention with a bag when out and about, but a routine lubricated type at home. They should also be informed how to obtain future supplies, what complications to look out for and whom to contact if any problems arise.
Frequency
The frequency of ISC varies according to individual's presenting symptoms and residual volume urine.
Guidelines for initiating ISC are currently lacking and most recommendations are between 2–6 times in 24 hours, so that the maximum volume drained is approximately 500 mls or as frequently as required to prevent urinary leakage in between catheters, but no more than 2 hourly (Vahr et al, 2013). However, while this is the rule of thumb, healthcare professionals need to take into account individual total bladder capacity compared to residual volume. For example, patient one's total bladder capacity equals 600 mls, which equates to 200 mls residual and 400 mls voided normally. The impact on their symptoms would be less than patient two, who also has a total bladder capacity of 600 mls, 400mls residual and only 200 mls voided normally. While they both have the same bladder capacity, the impact of the residual is greater on patient two than on patient one. This means that patient two would benefit from ISC more than patient one and may require it more often.
Frequency should be reviewed on a regular basis, as symptoms can improve but also deteriorate; for example, with long-term conditions such as MS.
Common problems associated with intermittent self-catheterisation
Although ISC is recommended as the ‘gold standard’ for bladder drainage, it does not come without its complications.
These include:
- Difficulty on inserting catheters: this could either be due to anatomical reason. For example, prolapsed or enlarged prostate in men or due to trauma, that is, urethral strictures or false passage from repeated catheterisations. False passage is rare. It occurs when a catheter has been inserted aggressively through a weak part of the urethra. Men may have difficulty inserting the catheter past the prostatic bed or through tense sphincter muscles. They should be advised to: relax; take some deep breaths and give a slight cough when they insert the catheter. If this fails, they should contact their specialist nurse as the prostate may be causing an obstruction. Women may have difficulty identifying the urethra
- Pain on insertion or removal can cause individuals to stop doing ISC completely. Pain may arise due to being too tense on insertion; older women may have vaginal atrophy, making the area sensitive. The catheter may trigger bladder spasms (anticholinergic therapy may help); this may also be caused when trying a different make of catheter or because there is not enough lubrication
- No urine drainage: the catheter may not be inserted into the bladder, but rather, inserted into the vagina instead
- Trouble removing catheter: the bladder mucosa sometimes gets sucked into the eyes of the catheter. In this situation, advise the individual to relax, wait a few moments, slowly rotate the catheter; this allows the mucosa to be released from the eyes. Coughing helps sometimes
- Bleeding: blood on the tip of the catheter during initial catheterisation is often common. This can be caused by the catheter scratching the lining of the urethra on insertion and/or removal. If bleeding is heavy or clots appear, the patient should seek medical help or contact their specialist nurse
- Leaking between catheterisations: this can be caused from stress urinary incontinence (weakness of pelvic floor), when the interval between catheters is too long or overactive bladder symptoms. These problems need an individual assessment and appropriate treatment plan, which may include reviewing fluid intake, frequency and technique of ISC. Anticholinergics may also assist.
However, the most common complication is UTIs. If recurrent infections occur, it is important to review the ISC technique, frequency, levels of hygiene and type of catheter being used. While the use of antibiotics is frowned upon, some of these individuals are high risk categories and may need appropriate use.
Conclusion
ISC is usually considered the ‘gold standard’; however, it is not without its drawbacks. It requires a competent professional, excellent in communication skills to identify the appropriate individual to undertake the procedure and instruct appropriately. They need to be able to alleviate the fears and concerns of the individual and put them at ease for the ISC to be successful. They need to be knowledgeable in the variety of intermittent self-catheters available and be motivating and supporting. If this is done correctly, then ISC is definitely the ‘gold standard’ for individuals to improve their bladder dysfunctions and quality of life, even with the complications outlined.
Key points
- Health care professionals must be aware of the indications for use of an intermittent self-catheter
- Health care professionals should be able to identify the advantages and limitations of intermittent self-catheters
- Health care professionals should be aware of the different types of intermittent self-catheters available
- Health care professionals should be aware of the significance of correct instruction of intermittent self-catheterisation and importance of regular follow up.
CPD reflective questions
- Identify individual patients that may be appropriate for intermittent self-catheterisation (ISC) and was this option discussed with them
- Reflect on individual patients seen and consider whether the intermittent self-catheter chosen was the most suitable or appropriate for that specific individual
- Contemplate whether the instruction of ISC followed current guidance or could be improved
- Indicate whether there is adequate follow up for individuals who undertake ISC


