In 2014, the Five Year Forward View (NHS England, 2014) announced the creation of new ways of delivering care that blurred the traditional boundaries between services. This road map included the development of out-of-hospital care, integrated working and patient empowerment strategies to help them manage their conditions, with the hope that this would enable services to be clinically and financially sustainable. The services within these new models of care were expected to utilise an integrated approach to deliver services to meet the needs of the local population.
To support this vision and as part of the local approach in Worcestershire, community services were integrated into neighbourhood teams (NT), with the last NT being formed in June 2018. These teams comprise registered nurses (general and mental health), healthcare support workers, physiotherapists and occupational therapists; some teams also include advanced nurse practitioners. At the time of writing, these teams were at different stages of development and had different priorities, according to the needs of the population.
During the process of NT establishment, staff roles and responsibilities changed to support this integrated approach. Further, in the preceding months, a significant number of senior and experienced staff had retired from the workforce, which led to the recruitment of more junior staff into band 6 roles to ensure that services could continue to be provided to high standards. It became apparent during the transition into NTs that many of the band 6 staff required additional support and education within their leadership role to enable them to develop their knowledge and skills. Thus, a clinical leadership programme was considered specifically for these staff. The staff identified to undergo this programme consisted of registered nurses (general and mental health) and allied health professionals (physiotherapists and occupational therapists).
This approach fitted well with Leading Change, Adding Value (NHS England, 2016), which aligns with the Five Year Forward View (NHS England, 2014) and provides a framework for nursing, midwifery and care staff to support the reduction in unwarranted variation and achieve the triple aim of ‘achieving better outcomes, better experiences and better use of resources’.
Programme development
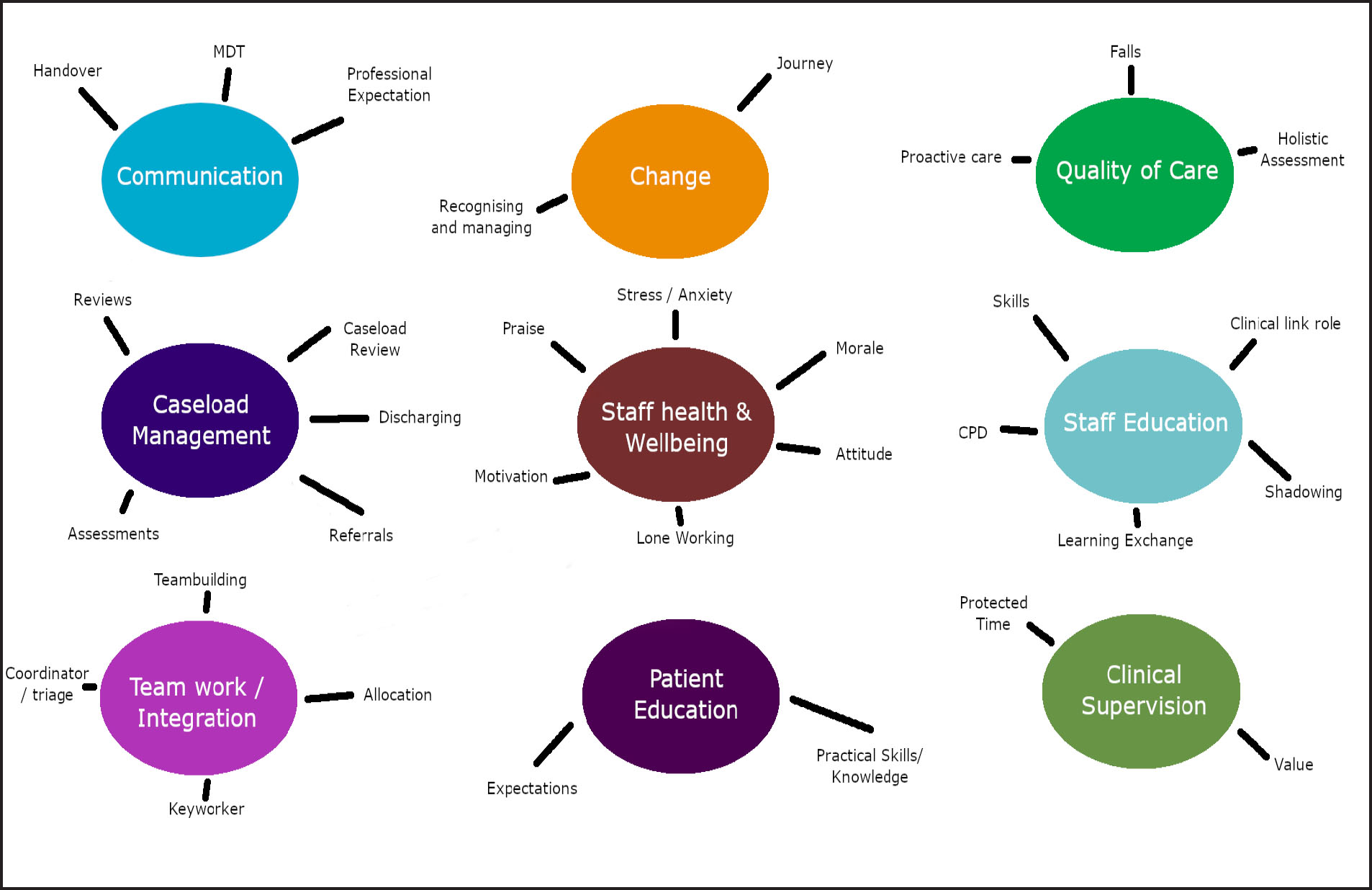
A skills analysis was undertaken across all the NTs in the county, and gaps in skills and knowledge were identified. This resulted in a discussion on the training needs within NTs between the service lead and NT leads. One of the priorities identified was the development and support of band 6 staff, due to changes in their role and the loss of significant numbers of experienced staff within the teams; clinical leadership was identified as the key need.
The NHS leadership framework (NHS Leadership Academy, 2011) was used as a starting point to identify the key components of the programme, as this resonated with the development needs that were identified, which included: managing yourself; managing a team and resources; improving quality of care and efficiencies within services; and change management. A draft programme outline was developed and shared with the service lead and NT leads; this led to further refinement of the programme outline to align with NT service needs. The workload of the NTs was increasing; hence, the capacity to release staff from the teams to attend the programme was also discussed. It was agreed that the programme would be a full-day session per month, with one delegate from each NT, and that the service could support two cohorts delivered concurrently.
During these discussions, it was identified that the programme could demonstrate how the service lead and NT leads valued their staff and could strengthen relationships between frontline staff and managers, which resulted in operational management involvement in the programme. The service lead committed to attend each session for approximately 30 minutes at the beginning to enable staff to share concerns, ideas, etc. (Box 1).
Objectives
The objectives of the programme were to provide education and support to enable staff in band 6 roles in NTs to:
The final programme was then devised within these parameters, with regular communication with the service lead and NT leads to gain agreement. During this time, venues and key speakers were identified and confirmed. The coordination of speakers required considerable time, and sourcing of venues was challenging at times, requiring some creativity in sourcing new venues. The budget for this came from the learning and development department of the Trust. The final programme was agreed in August 2018 and planned to commence in September. The allocation of selected staff to each cohort was completed in negotiation with the teams, to ensure that study leave was rostered without compromising service delivery. The programme details were then distributed to all nominated staff, and a process for recording attendance was agreed.
Programme implementation
The programme commenced in September 2018. The identified delegates for the programme were required to complete a survey on their personal resilience prior to the first session, as this would aid self-awareness of their resilience and support identification of their development needs. An appreciative inquiry approach was employed to identify development needs, which focused on a positive perspective. A SOAR (strengths, opportunities, aspirations, results) analysis tool was used. This tool differs from the commonly used SWOT analysis (strengths, weaknesses, opportunities, and threats) as it focuses on existing strengths, which are then built on to create a plan for positive change (Cooperrider, 2012).
The programme was delivered over 6 days, and the theme of each day was as follows:
Table 1 describes the topics covered on day 1. At the start of the programme, ground rules were established: it was agreed that the session was a safe space for open discussion and that discussions would remain confidential unless sharing of discussions or queries were agreed by the group, or if there were identified risks.
| Overview of the programme and objectives |
| Trust values |
| Emotional intelligence and appreciative enquiry |
| Robust leader reports, SWOT/SOAR analysis |
| Develop personal action plans |
| Circle of influence/the robust leader |
| Inclusion and the 9 protected characteristics |
SWOT: strengths, weaknesses, opportunities and threats; SOAR: strengths, opportunities, aspirations and results
Day 1 of the programme generated a lot of emotions. Some staff commented that they were used to exploring the needs of patients, carers and team members but not their own needs. Other comments were: ‘felt empowered’; ‘I didn't expect such an emotional day’; ‘keeping positive, feeling confident’; ‘identifying our strengths and looking at opportunities to improve’; and ‘thinking outside the box’.
Table 2 describes the topics covered on day 2. This day generated a lot of discussion and exchanges of ideas. What was becoming obvious was the need for staff to network and learn from each other. This was empowering and confidence building and stimulated creativity.
| Team SWOT analysis and challenges (from day 1) |
| Feedback from group discussions |
| e-rostering |
| Safer staffing, safe caseloads, caseload management |
| Performance management, sickness policy, probationary framework, appraisals |
| Delegation |
| Staff wellbeing |
SWOT: strengths, weaknesses, opportunities and threats
Day 3 was an intense day with lots of information for the groups to absorb. Some useful discussions were brought up, as well as some queries and suggestions for the presenters. One of the comments from the group was ‘[it was] helpful to see how integration is working in practice’ (Table 3). An evaluation was circulated among delegates after the day 3 session.
| National/local agendas |
| Contexts for change/managing change |
| Using information for service improvement |
| What information do you have about your service? How do you/will you use this? |
The day 4 session provided some practical information that the groups were unaware of and generated some ideas (Table 4). This included how the Trust supported staff as well as patients, and that the number of positive comments shared with the patient experience team by patients, carers and families about the service provided by the neighbourhood teams were significantly greater than any negative comments or complaints, which was motivating to hear.
| Medicine safety |
| Health and safety |
| Quality-driving lessons |
| Risk management and security |
| Patient experience (complaints/compliments/friends and family test) |
Exposing participants to trust-wide ‘corporate’ functions enabled them to view change through a wider lens and stimulated curiosity for creative thinking. One of the comments from the group was ‘[it is] useful to know who to contact for data to analyse caseloads’.
The day 5 session explored the information that the groups had received in the previous 4 days of the programme and used this to support problem solving, thinking differently and making changes. There were opportunities to share ideas and test conversations/scenarios in a safe environment with peer support (Table 5).
| Revisit SOAR/SWOT analysis from day 1 |
| Problem solving, creative thinking and leading change |
| Difficult conversations |
| Preparing for your presentation |
SWOT: strengths, weaknesses, opportunities and threats; SOAR: strengths, opportunities, aspirations and results
Delegates were asked to prepare a short presentation for the final day, which led to some anxiety, but was purposefully moving them on as leaders. Time was spent coaching them through how this might be approached. Comments from the group were: ‘Pig wrestling and how to problem solve was very useful’; ‘reassurance and useful advice’; and ‘by using a problem-solving approach in a structured way, one can solve anything’ (Lindsay and Bawden, 2019).
The day 6 session involved 15-minute presentations delivered by all staff attending the programme. These presentations described the ideas and action plans the staff had developed to support their team following completion of the SWOT analysis at the start of the programme. There was a range of presentation themes and delivery methods; some staff were very creative, and one included a YouTube video clip.
The line managers were invited to attend these presentations to provide support to their staff as well as the implementation of the action plans or ideas, as required. This also helped build the ‘team’, in a wider sense. Line managers reported that they noticed positive changes in terms of the delegates’ confidence. Some of the themes covered in these presentations were:
Outcomes and feedback
This in-house programme received positive evaluations from delegates and managers, who identified that all the programme objectives had been met.
Some of the comments from the delegates were as follows:
‘I realise I can take back some control!’ ‘Thank you for keeping me going through a really tough time’; ‘Has made me want to implement change’ ‘I feel I will be a more robust and dependable leader’
From the feedback, the elements of the programme most valued were:
Further, some changes suggested by delegates and managers included the following:
In the next installment of the programme, the following changes have been decided on: the next two cohorts are to include a greater proportion of AHPs, as well as staff from out-of-hours nursing teams; more AHPs are to be invited as speakers; and a session on motivating and retaining staff will be added.
Some other comments requested more information on managing challenging situations and having courageous conversations. Due to the time constraints of this programme, it was only able to deliver an overview of this subject, and delegates were signposted to the detailed training sessions available. Other learning from the programme was that it would be more beneficial to receive feedback after each session rather than at the mid-point and end of the programme. The continued involvement of operational managers in the delivery of the programme will provide valuable up to date information on national and local strategies that impact on the Neighbourhood Teams, such as the NHS Long Term Plan, Primary Care Networks and Sustainability and Transformation Partnerships (STPs).
Some of the comments received from managers were: ‘I have seen a change in confidence and positivity’; ‘Resulted in some really engaged, positive emerging leaders’; ‘Just, thank you for running the course’; ‘Really interesting to see the before and after’; ‘I think the investment with the course has really benefitted the individual and the team as a consequence’; ‘I feel this programme has made a real difference to staff being aware of the bigger picture; ‘A really well run, supportive leadership course!’
The feedback received from delegates and managers regarding this programme exceeded expectations. In addition to achieving the identified objectives, the delegates demonstrated changes in their behaviours and attitude when they were within their teams. Motivation in embracing change, encouraging team members and exploring new ideas with colleagues in other teams was greatly increased. The knowledge of the delegates increased regarding the changing picture of the NHS, how this affects the Neighbourhood Teams and staff emotional reactions to change, as illustrated in the ‘change curve’ (Kubler-Ross, 1969) and ‘Fisher's personal transition curve’ (Fisher, 2012).This enabled staff to support the change process more effectively and appeared to increase their resilience through increased positivity and emotional intelligence (Queen's Nursing Institute, 2018). At this stage, it cannot be determined if this positive change will be sustained; however, it is hoped that the planned follow-up workshops and group clinical supervision will enable these changes to realise long-term benefits.
The experience of the programme was shared with the associate directors and the director of nursing to enable the momentum of professional development and motivation to continue, as well as sharing the excellent ideas generated.
To continue this momentum, it has been agreed that further workshops or action-learning sets will continue and be supported by the service lead. Delegates will continue to have opportunity to work on service ideas and be encouraged to contribute to wider team development. The learning from setting up and delivering this programme has largely been that investing time and energy into listening and facilitating frontline clinicians to feel part of change is of great value. Workforce wellbeing is a key priority in sustaining today's NHS, and initiatives such as this, which are replicable with minimal outlay, are both rewarding to deliver and likely to bring tangible benefits to the work of the organisation. The NHS Long Term Plan (2019) identifies the benefit of continuing professional development in motivating staff and aiding staff retention, thereby enabling the best use of staff skills and experience to deliver care in a better way for patients.

