Over the last 30 years, health professionals have increasingly faced challenges posed by an ageing population, that presents with multiple conditions (Kingston et al, 2018). Clinical care in the UK, most often delivered by the NHS, is a finite resource. The overwhelming effect of ongoing demographic changes in the UK directly impacts capacity within the NHS, a situation that is being mirrored worldwide (Vetrano et al, 2017). These pressures are most often noticed through national newspaper headlines, featuring concepts such as ‘bed-blocking’, trolley wait breaches in emergency departments, emergency service call-out and attendance delays, a lack of social care capacity, restrictions to drug funding imposed by National Institute for Health and Care Excellence (NICE) and cancelled operations (Iacobucci, 2017). Thus, this finite service seems to face infinite demands.
Alongside these substantial demographic changes is the challenge of considerable staff shortages across NHS provision, which are predicted to rise to in excess of 250 000 by 2030 (King's Fund, 2018). These shortages impact on the full range of clinical roles, with an estimated 40 000 nurse vacancies (Royal College of Nursing, 2017) and a reported fall in GP numbers by 450 full-time equivalents (FTE) between September 2017 and 2018 (Iacobucci, 2019). A further challenge is the ongoing impact of economic recession, which has led to considerable and wide-ranging austerity measures (Stuckler et al, 2017). Healthcare expenditure is often the first to experience funding cuts, which impacts on core services but, in addition, there has been a stark reduction in community support services (Age UK, 2018). Indeed, Mencap (2016) reported a 33% decrease in community-based support services for older people and those with learning disabilities.
The NHS Long Term Plan (LTP) (2019) aims to direct care provision over the next 10 years and firmly focuses on the need to ensure that patients remain within primary care; keeping the patient at home with hospital admission avoidance and shortening lengths of hospital stays as much as possible are central to coping with unprecedented demand. Indeed, the LTP (NHS, 2019) sets out a strategy, supported by new money, delivered across a number of primary care networks (PCNs). PCNs comprise multidisciplinary teams (MDTs), equipped to empower patients to concord with mutually agreed, ambitious plans of care, aimed at maintaining health for as long as possible.
For such plans to be effective, partnership working between health professionals (HPs) and their patients is fundamental. Clear information, shared decision-making, effective care planning and realistic goals for self-management will need to be at the core of care provision across the NHS (NHS, 2019). Additionally, a concordant relationship between patient and HP is essential. Such relationships will be underpinned by trust and negotiation; indeed, a relationship of equals with shared goals rather than a paternalistic approach (Morley and Floridi, 2019). Theories of person centredness have been espoused for a long time (Ballint, 1957), but are still not consistently in place (Bhattacharyya et al, 2019).
Concordance is based on the sharing of information and the development of negotiated and agreed goals, in contrast to compliance, which requires adherence to a dictated plan with little or no negotiation. By its nature, compliance is often short-lived, with patients quickly demonstrating non-adherence to the plan set (Bissell, 2004). In order to achieve the goals of a concordant relationship, the LTP (NHS, 2019) elaborates that this will be underpinned by the implementation of seamless technology to support information sharing and to fully equip patients to engage with informed and shared decision-making with their HP.
Challenges to concordance
On occasion, despite HPs' best efforts to share information and develop a relationship of ‘equals’ with patients, some patients still fail to concord (Seligman, 1975; Hewison, 1995; Morden et al, 2012; Felzmann, 2018). Apparent nonconcordance may occur despite best efforts to engage the patient in self-management and to share decision-making.
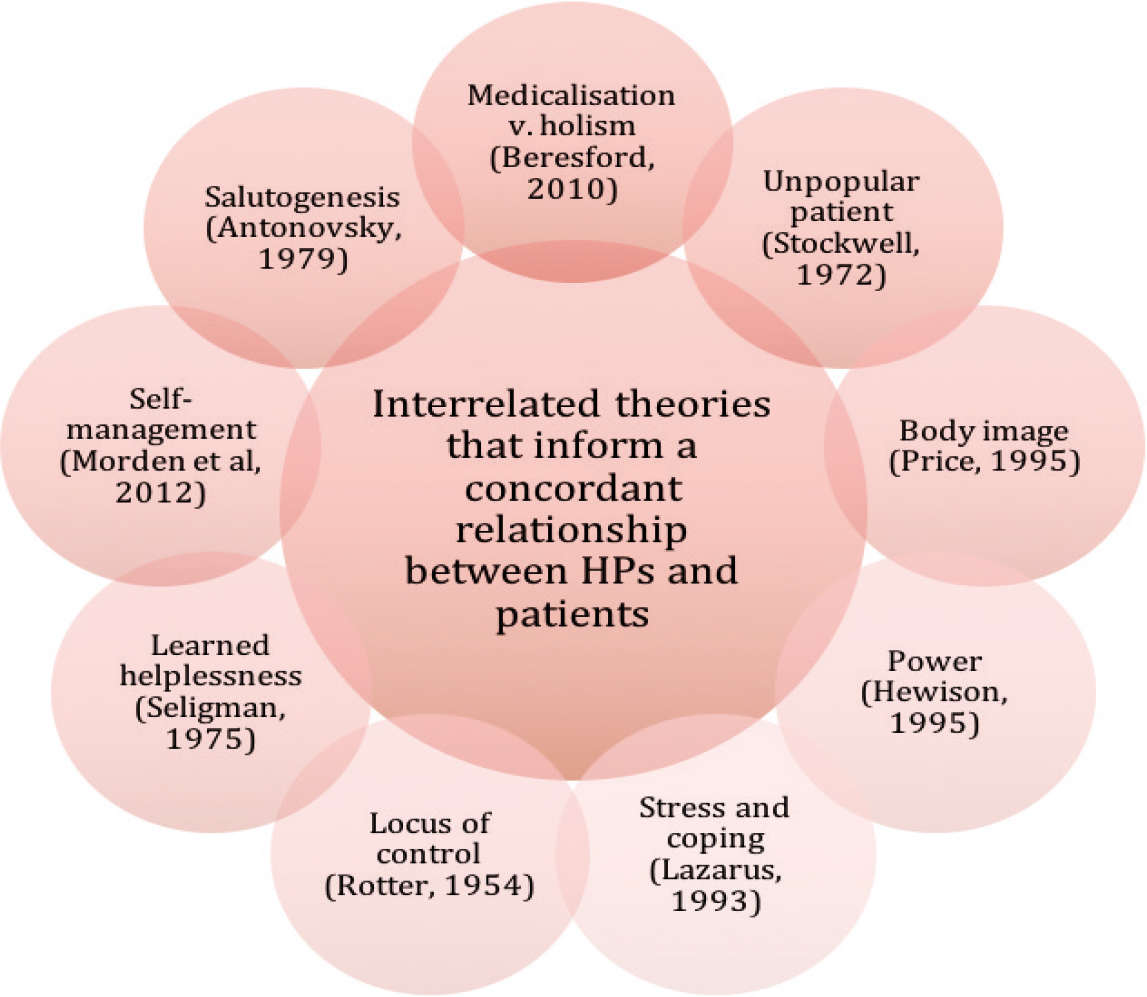
There are a range of theories that attempt to explain this conundrum and may well inform more effective approaches to engaging certain patients as partners in care. These theories, as a minimum, serve to enhance understanding of the HP–patient relationship but, at times, may go some way to explain the actions and reactions of each party within this complex relationship. Understanding these theories may also infl uence the approaches adopted by HPs. Each of these theories is presented here, alongside suggestions for potential alternative approaches to care delivery (Figure 1).
Medicalisation and holism
The term ‘medicalisation’ describes a ‘reductionist’ philosophy, most often linked with a medical approach to care delivery, which is underpinned by an aim to describe and define the disease process (Ahn et al, 2006; Beresford, 2010; Gray et al, 2015). Indeed, the aim of medicalisation is to develop an understanding of the management of the disease process. However, medicalisation is often criticised for focusing on the minutiae of disease and disease prevention but lacking an insight into the ‘bigger’ picture, which includes its impact on the patient (Ahn et al, 2006). Gray et al (2015) acknowledged a range of new pressures to ‘medicalise’, including that driven by the patient as an ‘expert’, government programmes such as the Quality and Outcomes Framework, the ‘industry’ of lifestyle medication and the lowering of treatment thresholds and routine screening. They purported that ‘medicalisation means medication for millions' (Gray et al, 2015:7), with lowered thresholds for a range of diseases.
The risk of a medicalised approach is that the condition or ‘disease’ is disassociated from the patient and their experiences (Beresford, 2010). This problem is intensified with an increasing reliance on evidence-based medicine (EBM), rather than the effectiveness of treatment and management within a real-life context (Beresford, 2010). Beresford (2010) warned that advice from HPs who adopt a medicalised approach may be so specific that any application to a real patient may lead to harm or disengage the patient. This effectively sums up the traditional medical model, where dialogue may be paternalistic and imposed rather than negotiated. In such a situation, patients do not perceive themselves as equal partners in a relationship. An example of such a situation would be the implementation of an aggressive and challenging management plan for a patient with an advanced diagnosis of cancer without negotiating the patient's priorities for their future care.
In contrast to the medicalised model, holism represents an opposite approach, emphasising the centrality of the patient within the disease process and the need for the whole person to be accounted for within the delivery of care. In order to optimise concordance, it is suggested that holism should be the goal of patient-centred care delivery, and this is effectively summed up by Beresford (2010:721) as follows:
‘…. looking at the patient and disease as a whole rather than focusing on interactions at cellular level’
Historically, the first truly holistic practitioner in nursing was Florence Nightingale, who emphasised a need to focus care on the whole patient, with an awareness of the influence of environmental factors on health and recovery (Dossey, 2010).
Contemporary issues within healthcare systems question whether the approach to care delivery and nursing are truly holistic, especially since care is most often delivered within specialist silos, with an emphasis on a single disease, despite the growing prevalence of multimorbidity (Smith et al, 2011). The themes stressed within holism include the centrality of the patient as a whole, positioned at the centre of the care dialogue and at the heart of person-centred care. Such themes, however, are not without their challenges within an in-patient setting, as patients are quickly discharged, fast tracked or transferred. This minimises the opportunity for meaningful dialogue, goal setting and an effective holistic approach to care delivery.
The Unpopular Patient
In 1972, Stockwell published a seminal text entitled ‘The unpopular patient’. This research explored interpersonal relationships between the nurse and their patient and was undertaken in hospital wards. The focus of Stockwell's (1972) study was the interaction between the patient's and the nurse's personalities. It aimed to investigate the meaning behind why some patients were classified as ‘difficult’ by nursing staff, and described these ‘unpopular’ patients as those ‘… whom the nursing team enjoys caring for less than others' (Stockwell, 29172:11).
Stockwell (1972) found the impact of this classification on patient care to be surprising, with results identifying a middle group of patients who were categorised as being neither popular nor unpopular, but who were nonetheless deprived of attention. At the time, this research was extremely contentious and challenged the widely held view that nurses were non-judgmental in their care. Although now dated, Stockwell's (1972) research remains relevant and, when most nurses consider the care that they deliver, they will be able to identify those to whom care is more easily delivered.
More recently, the description of patients as ‘heartsink’ was coined within general practice (O'Dowd, 1988), mirroring Stockwell's (1972) ‘unpopular patient’. ‘Heartsink’ was used to refer to patients who caused their HP to feel ‘heartsink’ (Moscrop, 2010). Ellis (1986:318) had previously described such patients and a feeling as ‘dysphoria’, describing it as:
‘… the feelings felt in the pit of your stomach when their (the patients') names are seen on the morning's appointment list’.
O'Dowd (1988) described such patients as being thought of as dissatisfied, manipulative, demanding and frequent complainers but, on closer inspection, found that they actually represented a disparate group of complex patients. The views expressed by O'Dowd (1988) were amended during ensuing years (Moscrop, 2010).
The ‘heartsink’ theory displayed many similarities to Stockwell's (1972) ‘unpopular patients’ and the revelations about nurse attitudes. Studies demonstrated that ‘heartsink’ patients may experience ineffectual management of their condition as a result of the impact of ‘heartsink’ on the HP concerned, who may be frustrated and act in an unprofessional manner during clinical contact (O'Dowd, 1988; Moscrop, 2010).
These studies suggest that patients may fall into the category of being difficult without being aware of such marginalisation or the impact that such a label may have on their care (Stockwell, 1972; O'Dowd, 1988). More recent studies have also had similar findings (Bass, 2016). This evidence suggests that HPs need to be aware of any prejudices that they hold, in order to ensure that all in their care receive the same level of care.
Body image
All people have a personal perception of their body; this is the picture of their body that they hold in their minds and ultimately define how they see themselves (Schilder, 1935). Changes to physical appearance, which may be as a result of illness or disease, have an impact on personal identity and may displace one's view of oneself (Price, 1999; 2000). Price (1999) worked extensively in the area of body image and claimed that the initial steps to correct a distorted body image, early in an illness trajectory, may be successful but, often, as the disease progresses, the effectiveness of such interventions diminishes. As a result, the illness actually stigmatises the person due to their changed appearance and general loss of bodily control (McIntyre, 1995; Price, 1999). Price (1995:180) described altered body image as:
‘a state of personal distress, defined by the patient, which indicates that the body no longer supports self–esteem, and which is dysfunctional to individuals, limiting their social engagement with others'
Altered body image is extremely common in palliative cancer care and may result from a person's diminished ability to manage the impact of their illness or as a result of the reactions of others to their condition (Cook, 1999).
Changes to body image affect a range of patients, including those who have required surgery and those with wounds requiring visible dressings. Patients requiring lower limb dressings are a group in which concordance to treatment may be impacted by the appearance of dressings (Williams, 2010); a negotiated approach to ensure concordance will result in the best response from the patient. It is important that the HP reassures the patient and aims to minimise the impact of the condition on the patient's perception of their body image.
Power in the HP–patient relationship
The HP–patient relationship is not necessarily one of equals (Beck, 1997; Henderson, 2003; Barry and Edgman-Levitan, 2012), and this is a factor that affects the effectiveness of any ensuing dialogue.
Power in the nurse–patient relationship was explored by Hewison (1995), who analysed and explored the language used during nurse–patient interactions, concluding that nurses used language to exert power over their patients—a behaviour that was generally accepted as normal. Despite the accepted ‘normality’ of this, such behaviour presented a barrier to the development of a collaborative nurse–patient relationship and often prevented open and meaningful communication. Hewison's (1995) study confirmed that most nurse–patient interactions were trivial, routine and task-related. This assumption was corroborated by Henderson (2003) and McCabe (2004), who also found that the impact of power in the HP–patient dialogue served to limit disclosure and thus affected the agreement of appropriate interventions.
More recently, Corless et al (2016) explored the imbalance of power between the patient and HP and evidenced the negative impact of such dialogues on the patients' experience of care. The nurse's interactions are often workload-driven rather than being intentionally aimed at distorting the quality of care delivered. The impact on the patient's experiences of care are negative as a result. HPs need to be conscious of their interactions with their patients to ensure that a power relationship is avoided. Corless et al (2016:20) stated that:
‘Nurses may possess a number of attributes that place them in a powerful position in comparison with their patients. These include professional status, professional knowledge, being free of pain and fear, and being in a standing position rather than lying in bed’.
Stress and coping
Theories of stress, coping and health are often derived from Lazarus' (1993) original transactional model, which was developed in response to an increasing interest in the area of stress in the 1960s and 1970s. Lazarus (1993) believed that responses to stress depended on the meaning that an individual attributed to the stressful stimulus, and thus affected both health behaviour and coping. Lazarus (1993) proposed that coping efforts depending on primary and secondary appraisals of an impending stressor.
According to Lazarus (1993), primary appraisal referred to an assessment of the threat that a situation poses to an individual. Secondary appraisal referred an individual's assessment of the resources available to them to cope with the stressor. These responses could be a problem-focused strategy, such as information seeking, or an emotionally focused strategy, such as changing personal thinking about a situation, avoidance and denial.
Application of the transactional model supports the positive benefits of social support for an individual with regard to wellbeing and health. Indeed, social support is important, although Schwarzer and Leppin (1991) suggested a more complex interaction with social support mediating the effects of illness and directly affecting illness. The transactional model (Lazarus, 1993) underpins the need for support mechanisms for patients, to empower them to cope with the challenges that their condition and treatment present. This model also explains a person's responses to multiple stressors, whereby secondary appraisal may, in fact, reinforce a belief that a person can no longer cope and that they have no more strategies to cope with the stressors presented.
Models that identify the benefit of social support, against a backdrop of diminishing resources (Gerst-Emerson and Jayawardhana, 2015), present many challenges to HPs. Indeed, austerity has impacted many of the resources previously used to support more isolated patients and, with loneliness impacting on the health of many patients, not least older adults (Age UK, 2018), referral pathways are more limited, and solutions are harder to achieve.
Locus of control
Many studies have aimed to explore personal characteristics in order to establish why patients act and react in a certain way; one such psychological theory is known as ‘locus of control’ and was expounded by Rotter in 1954. Rotter (1954) aimed to describe the degree to which a person believes they can control the events in their life.
A person's locus, or place, is described as being either ‘internal’ or ‘external’. When a person's locus of control was internal, they held a belief that they are in control of their life. In contrast, those whose locus of control was external felt that they and their decisions were controlled by factors that were beyond their control (Rotter, 1954).
The theory of locus of control can have a significant impact on a person's ability to engage in self-care and whether they feel that they are able to make effective changes in order to improve their health outcomes. Indeed, those with an internal locus of control tend to cope well with their diagnosis and are often keen to engage with self-management, believing that this will improve their outcomes. In contrast, those with an external locus of control prefer their condition to be ‘managed’ by their HP and are reluctant to self-manage. Indeed, a study by Musich et al (2019) demonstrated the impact of an internal locus of control in their study about the experiences of pain in older adults. Their analysis evidenced that those with an internal locus of control had lower pain severity, reduced chronic opioid use and increased physical functionality.
An awareness of a patient's locus of control may enable the HP to negotiate plans of care and provide the level of support required, as enhanced psychological and emotional support may well be required for those whose locus is external.
Learned helplessness
Another personal characteristic relevant to person-centred care and the effectiveness of consultations is ‘learned helplessness’. This trait was identified by Seligman (1975) to describe why some people, when faced with a negative situation, tend to behave helplessly and remain passive, despite having an opportunity to correct the situation.
Seligman (1975) adopted the phrase ‘learned helplessness' to describe a belief that events were out of an individual's control. In addition to the negative expectations held by those with learned helplessness, Seligman (1975) identified that such feelings were often accompanied by feelings of low self-esteem and persistent failure.
Smallheer et al (2017) further explored the impact of learned helplessness on depressive symptoms following myocardial infarction, demonstrating a statistically significant relationship between learned helplessness and depressive symptoms and suggesting that higher self-reported levels of learned helplessness were linked to the reporting of increased depressive symptoms.
Learned helplessness results when a person is repeatedly unsuccessful in dealing with situations that are stressful or challenging. This impacts on motivation, cognition and emotions, minimising the expectation that things will improve as a result of personal action and, thus reducing future attempts to react to an unfavourable situation (Seligman, 1975; Smallheer et al, 2017). For HPs to focus their consulting approach to effectively engage, encourage and motivate patients, it is vital that they understand patients who exhibit learned helplessness. Goal setting, motivational interviewing and effective person-centred approaches may serve to minimise learned helplessness.
Self-management theory
The theory of self-management is embedded in policy and practice (Department of Health and Social Care (DHSC), 1991; 2001; NHS, 2019) and is defined as care directed and led by the patient (Morden et al, 2012). The term ‘self-management’ is key to a patient-centred health system and fundamental to the effective management of long-term conditions (LTCs) (DHSC, 2005; NHS, 2019). The theory of self-management is underpinned by a patient's motivation to engage in their care and is linked to the theories of locus of control (Rotter, 1954) and learned helplessness (Seligman, 1975).
The elements that underpin the adoption of self-management are encapsulated in the theory of self-determination, initially described by Deci and Ryan (2000). Self-determination focuses on two types of motivation for health: controlled and autonomous. People who demonstrate ‘controlled motivation’ undertake interventions for extrinsic reasons, for example, for a specific reward or to make others happy. In contrast, those with ‘autonomous motivation’ act for intrinsic reasons, acting to benefit themselves. Autonomous motivation has similarities to internal locus of control (Rotter, 1954), can predict positive changes in health and is key to self-management (Deci and Ryan, 2000).
Alongside self-determination are social learning theory or self-efficacy (Bandura, 1977); this theory is also implicated in a patient's positive motivation to engage in self-management and focuses on an individual perceiving that they are able to undertake the behaviours necessary to improve their health. Again, these behaviours are predictive of self-management (Bandura, 1977; Skinner et al, 2003). Indeed, a personal belief in the ability to improve health outcomes is often predictive of the success of treatment interventions and impacts on their compliance with such regimes (Deci and Ryan, 2000). In contrast, controlled motivation, as with an external locus of control, may see patients disengaging, preferring their HP to manage their condition for them.
Self-determination underpinned by autonomous motivation and self-efficacy are predictive of self-motivated patients, who are keen to optimise their health outcomes and engage in self-management, underpinned by the belief that improved outcomes are achievable. However, those with controlled motivation and an external locus of control may need a plan of care that is more directive, alongside motivational interviewing to inspire some degree of concordance to plans.
Salutogenesis
Antonovsky (1979; 1987) contested the widely held biomedical model of health and proposed a new ‘continuum model’ of health model. The model describes that each person is positioned, at any point in time, on a health/disease continuum (with health termed ‘salutogenesis’ and disease termed ‘pathogenesis').
Antonovsky (1987) stressed the importance of the person's ‘sense of coherence’, a unique attribute held by all individuals. ‘The sense of coherence is an individual's approach to the world and to what extent they perceive it as ‘comprehensible, manageable and meaningful’ (Johnson, 2004:420). The sense of coherence, Antonovsky (1987) felt, was significant in an individual's movement toward the health end of the continuum when faced with a particular stressor. Those with a strong sense of coherence would understand the challenge, be motivated to cope and would apply the resources required (Antonovsky, 1987). Again, similarities can be seen with an internal locus of control and self-efficacy (Rotter, 1954; Bandura, 1977).
Antonovsky (1979) also expounded the importance of something he termed ‘generalised resistance resources’ (GRRs). He described these as the properties necessary to enable a person to cope, to view the world as making sense, cognitively, instrumentally and emotionally. GRRs were described as biological, material and psychological factors that make it easier for people to see their lives as consistent, structured and understandable. GRRs include money, knowledge, experience, self-esteem, being loved, healthy behaviour, commitment, social support, cultural capital, intelligence, traditions and view of life (Antonovsky, 1979). Antonovsky (1979) felt that sufficient and appropriate GRRs facilitated movement towards the health end of the continuum. Antonovsky (1979; 1987) proposed that if a person has some or all of these GRRs at their disposal, they would have a better chance of coping with the challenges of life (Antonovsky, 1979; 1987; Lindstrom and Eriksson, 2005; 2006).
Research demonstrates that in all age groups, socioeconomic backgrounds and cultures, those who demonstrate a strong sense of coherence experience better perceived health, improved mental wellbeing, healthier ageing and enhanced quality of life (Antonovsky, 1987; Lindstrom and Eriksson, 2006). Conversely, those with a weak sense of coherence experience poorer perceived health and low mood (Antonovsky, 1987; Lindstrom and Eriksson, 2006). Clear links can also be seen with locus of control (Rotter, 1954), learned helplessness (Seligman, 1975) and self-management theories (Morden et al, 2012). Salutogenesis has obvious implications for the adoption of self-management strategies and the development of a concordant relationship. It is clear that patients who lack a sense of coherence and GRRs, are often those who are unable to motivate themselves to self-care
Discussion
The psychological theories presented all have the potential to impact the ability of patients to self-manage their health conditions. Indeed, the success of the LTP (NHS, 2019) and the ability of the NHS in the 21st century to cope with unprecedented demands is predicated on a high proportion of patients engaging in self-management, supported by their HP. As can be seen in the theories described, many factors can impact a person's belief that self-care can be effective; this may be based on previous failures, negative feedback, poor understanding of what is required or a lack of GRRs (Antonovsky, 1987).
Patients with an internal locus of control (Rotter, 1954), a strong sense of coherence (Antonovsky, 1987), demonstrated self-efficacy (Bandura, 1977), problem-focused strategy (Lazarus, 1993) and autonomous motivation (Deci and Ryan, 2000) are, most probably, those who are easy to motivate to self-manage. They are enthusiastic, engaged and perceive that their outcomes will improve. Such patients adhere to advice, engage with shared care and investigate their condition.
In contrast, patients with an external locus of control (Rotter, 1954), a poor sense of coherence (Antonovsky, 1987), an emotionally focused strategy (Lazarus, 1993) and controlled motivation (Deci and Ryan, 2000) question their ability to engage and lack agency in determining their health outcomes.
It should be noted that the psychological theories mentioned here are not necessarily permanent. A patient who, in the past, has tried and failed to manage their condition(s) may feel demoralised and less likely to engage in the future. However, encouragement and motivation from HPs can re-motivate patients, invigorating them to re-engage with their condition, participate with their shared care plan and achieve incremental negotiated goals.
‘Patient activation’ is a term that describes ‘the extent to which individuals are able to manage their own healthcare’ (Magnezi et al, 2014). Hibbard et al (2004) designed a simple model entitled the Patient Activation Measure (PAM) to assess a person's confidence in engaging with self-management. Results ranged from not believing they play any role in self-care to being actively engaged in health behaviours. Many studies have evidenced that an initial focus on enhancing a person's self-assessed ‘activation’ level may result in improved responses to self-management interventions over time (Deen et al, 2011; Shively et al, 2013).
Challenges that may affect practitioners' success in promoting self-management include demographics, the workforce crisis and austerity, as well as the preparedness of practitioners to handover the ‘control’ of LTC management to their patient. Healthcare is an equal partnership and there is a need to acknowledge that clinicians do not hold all of the answers. HPs are often confronted by a ‘Google’ population of patients; health information is one of the most frequently searched topics on the internet (McMullan, 2006), and health-related websites have a considerable influence on the behaviour of website users (Turan et al, 2015). Patients often consult their HP already armed with a level of web-based information, albeit often of dubious quality or relevance, but this in itself is patient engagement and should not be discouraged. It is the role of HPs to guide patients to appropriate evidence-based websites and to not feel threatened by such information-seeking behaviours, as these are classified using PAM as active engagement with self-management behaviours (Hibbard et al, 2004).
Conclusion
The psychological theories presented can enhance or diminish person-centred care, communication between the HP and the patient during their consultation and the patient's ability to engage concordantly with self-management. Each theory poses its own challenges which may lead to mismatched goals and affect the patient's expectations of improved self-management. The HP is often the key to providing appropriate motivational goals for patients.
HPs must recognise these underpinning theories within their patient population and to vary their approach accordingly, in order to optimise outcomes. Adopting the right approach for the patient can affect their self-belief and permit patients to see that changing their mind-set might make a difference to their outcomes. Motivational interviewing, an awareness of the patient's activation level, a stepped approach to shared care, providing staggered, clear information over time, celebrating small successes and planning a gradual handover of health objectives may all well motivate those who lack the outward signs that they are prepared to fully engage in shared care.

