References
Aerosol-generating procedures in home care
Abstract
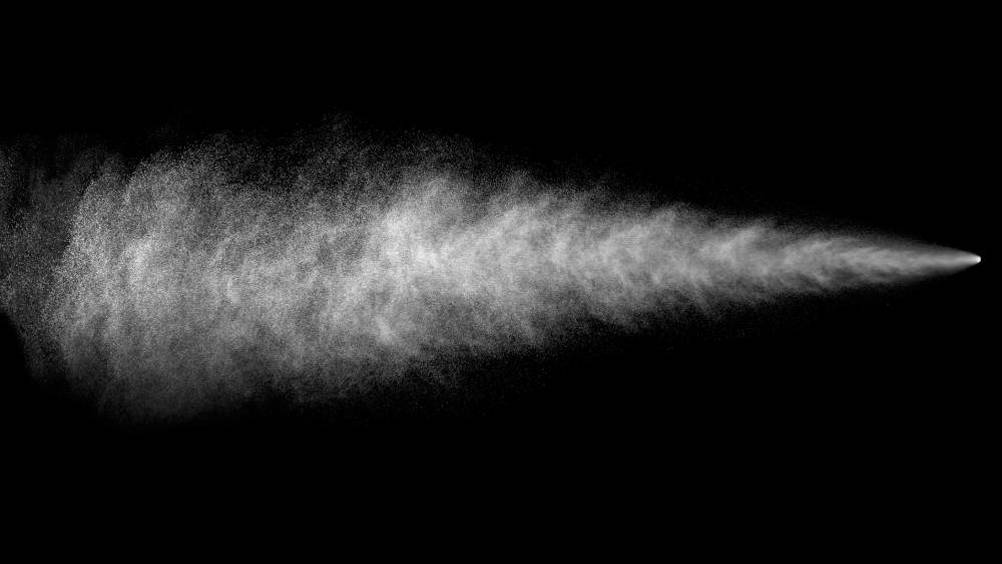
COVID-19 has changed the landscape of healthcare in the UK since the first confirmed case in January 2020. Most of the resources have been directed towards reducing transmission in the hospital and clinical environment, but little is known about what community nurses can do to reduce the risk when they nurse people in their own homes? This article looks at what COVID-19 is, how it is spread and how health professionals are at an increased risk from aerosol-generating procedures (AGPs). There is also a discussion on the benefit of mask usage. It defines what AGPs are, which clinical procedures are AGPs, including ones performed in the community setting, and which identified clinical practices that have been mistaken for AGPs. There is also a discussion on the suitability of performing cardiopulmonary resuscitation (CPR). It also describes how to reduce the risk by the use of full personal protective equipment (PPE) and other strategies when AGPs are performed in a patient's home. It ends with general advice about managing the risk of COVID-19 transmission with patients in their homes.
The first case of COVID-19 in the UK was diagnosed on 31 January 2020 (Tang et al, 2020) and, since then, this viral infection has dominated healthcare, the country and the world at large. Several studies have been published about the disease and how to manage patients infected with it, but the vast majority of them are about hospital and in-patient care. However, the majority of patients with COVID-19 are not admitted to hospital (UK Government, 2020a). This article looks at the risk of cross-infection of COVID-19 in patients' own homes, especially from aerosol-generating procedures, and what can be done to reduce this risk.
COVID-19 is a novel, or new, coronavirus (World Health Organization (WHO), 2020). Coronaviruses are named after the crown-like spikes that cover their surface (Centers for Disease Control, 2019), and the group includes the Middle East respiratory syndrome (MERS) virus, severe acute respiratory syndrome (SARS) virus and the influenza virus that causes the common cold (CDC, 2019). Similar to other coronaviruses, SARS-CoV-2, the causative agent of COVID-19, is a respiratory virus that is spread via respiratory droplets, from coughing and sneezing, and being in close proximity (within 2 meters) presents the greatest risk of transmission (Master and Gerrard, 2020).
Register now to continue reading
Thank you for visiting Community Nursing and reading some of our peer-reviewed resources for district and community nurses. To read more, please register today. You’ll enjoy the following great benefits:
What's included
-
Limited access to clinical or professional articles
-
New content and clinical newsletter updates each month

