Providing a coordinated and strategic approach to the assessment, treatment and management of chronic wounds is central to the provision of effective nursing practice. Approximately 2.2 million patients are living with a chronic wound in the UK (Guest et al, 2015; 2017; 2018), and improving the assessment of chronic wounds is a national priority (NHS England, 2018a). From the patient perspective, there are demonstrable negative consequences of living with a wound, including the psychological and emotional impact associated with increased pain, reduced mobility and physical impairment owing to the wound itself (Fearns et al, 2017). Patient quality of life (QoL) is also impacted by the clinical complexities associated with delayed healing and extended hospital care (MacDonald, 2009).
Wound care in the UK is estimated to cost the NHS £5.3 billion per year (Guest et al, 2015). On the current trajectory, these costs are expected to rise significantly, due to an increase in the number of people living with a wound and an ageing population with comorbidities, which increase the possibility of developing complex wounds that are difficult to heal (Guest et al, 2017). Data obtained from a retrospective cohort analysis of 2000 patients from The Health Improvement Network (THIN) database found that, from approximately 11 200 wounds, 48% were defined as being chronic (Guest et al, 2015). The number of people living with a chronic wound has led to inconsistencies in care across healthcare services. Gray et al (2018) conducted a survey across eight services within five community trusts in England, using data obtained from a population of 3179 patients with a total of 5632 wounds. The results showed marked variances in wound care treatment strategies, highlighting inconsistencies in care and the heightened demands and challenges placed on health professionals dealing with wound care.
Chamanga et al (2014) found that wound care in the community accounts for approximately half of nursing caseloads and, more recently, the Carter review (NHS England, 2018b) acknowledged that 51% of community nursing time was dedicated to wound care. Guest et al (2015) highlighted that leg ulcers (unspecified, venous, arterial and mixed) accounted for over 30% of all wounds, and fewer than half were associated with healing within a 12-month period of care. Venous leg ulcers (VLUs) alone were found to account for approximately 2.1 million patient visits per year (British Association of Dermatologists, 2017).
Need for evidence-based wound management
The Carter review (NHS England, 2018b) encouraged the implementation of evidence-based practice as a means to improve outcomes, but added that a large proportion of trusts ‘do not capture basic information on wound care, including the number of patients with wounds, wound types, treatment plans or, most critically, wound healing rates' (NHS England, 2018b: 14). Without accurate data being captured in this field of high clinical demand within the community, the opportunity to implement improvements and the ability to demonstrate their impact on national CQUINS and local quality-improvement programmes will be limited (Coleman et al, 2017; NHS England, 2018a).
The NHS acknowledged that implementing positive change in practice needs to be built on a commitment to change and relationships, rather than just compliance, and through a shared purpose, rather than transactions. This is built on relationships that drive the sharing of ideas and embracing change (Bevan and Fairman, 2014). Awareness of evidence-based practice does not always translate into implementation and sustained change due to multiple factors that may not be within the control of those delivering care (Rangachari et al, 2013; Grothier, 2018). Staff engagement is key in driving organisational improvement and maximising patient experience, particularly during times of austerity and increasing emphasis on performance (NHS England, 2018b). Empowering clinicians in the community setting with an evidence-based treatment protocol could potentially lead to significant improvements, but only if these can be measured and demonstrated (Coleman et al, 2017). Given the significant burden posed by chronic wounds, the implementation of evidence-based strategies in clinical practice is crucial to limiting the health and financial implications associated with wound management.
Clinical evidence supporting improvements in standard of care and cost with UrgoStart
Robust clinical evidence has demonstrated significant improvements in wound healing rates with the UrgoStart treatment range against a comparator, in combination with recognised standards of care for non-infected diabetic foot ulcers (DFUs), VLUs and mixed aetiology leg ulcers (MLUs) (Meaume et al, 2012; 2017; Münter et al, 2017; Edmonds et al, 2018), and the product treatment range was also endorsed by the National Institute for Health and Care Excellence (NICE) (2016).
A double-blinded randomised controlled trial (RCT) by Meaume et al (2017) demonstrated significant improvements in patient-reported QoL, including reductions in pain, discomfort and anxiety, in addition to improved clinical outcomes. Therefore, improving healing rates may significantly reduce the emotional and social burden associated with these wounds (Meaume et al, 2017).
Cost modelling (NICE, 2019a) has generated a potential savings estimate of £541 per patient when VLUs are treated with the UrgoStart treatment range, with a potential total saving of over £20 million a year (NICE, 2019b) for the NHS when used instead of a non-interactive dressing.
Project aims and objectives
Supported by the local tissue viability service, a community district nursing team initiated a quality-improvement project with the aim of incorporating the above NICE guidance for the UrgoStart treatment range within its wound management practice.
The project aimed to evaluate the introduction of an evidence-based wound care pathway (Figure 1) for the management of chronic wounds, particularly leg ulcers. These wounds were assessed as appropriate for early intervention with the UrgoStart treatment range as the primary dressing in conjunction with the usual standard of care. Any wounds with signs of infection were excluded and treated with antimicrobial therapy.
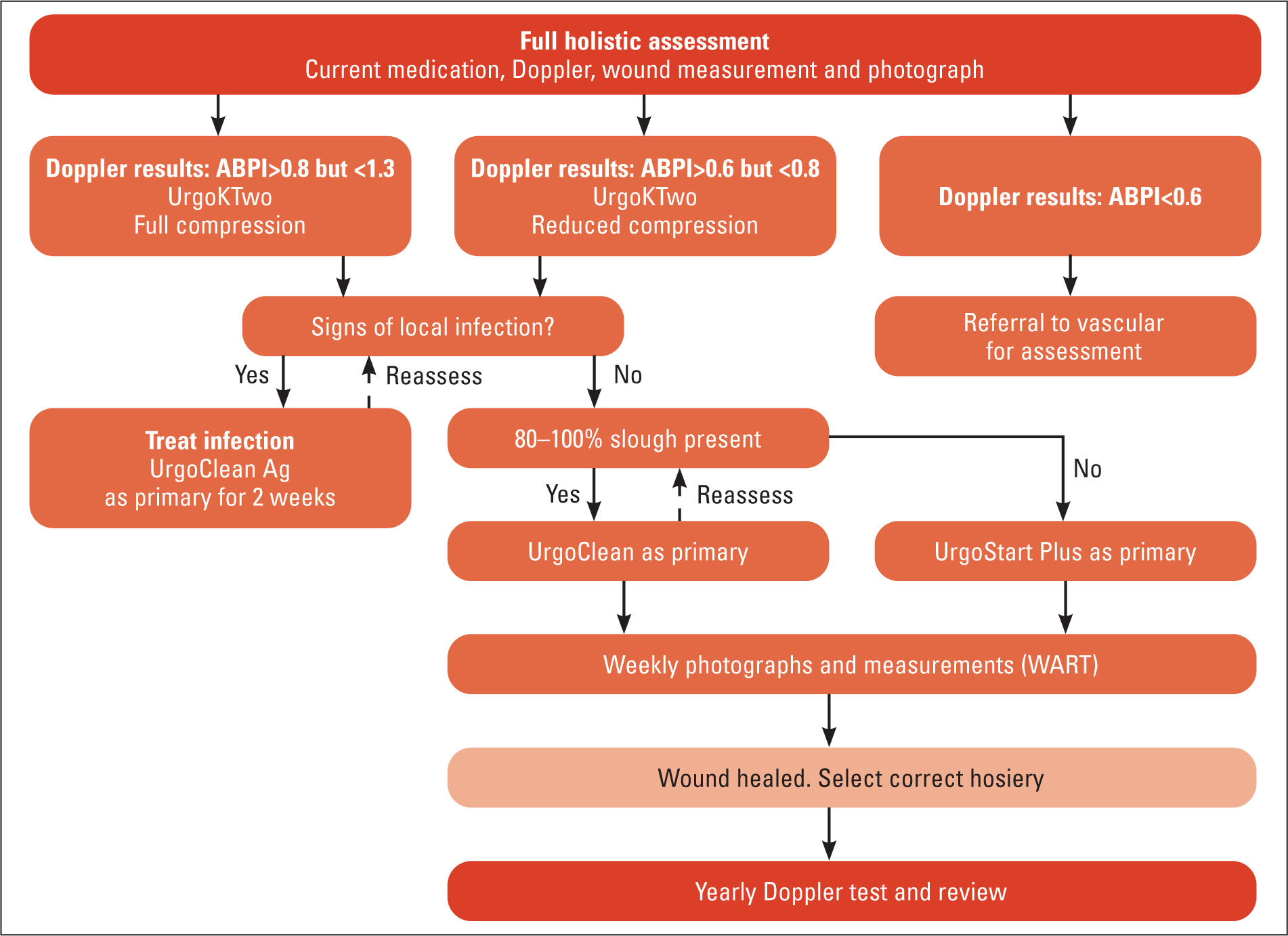 Figure 1. Bellingham district nurse leg ulcer pathway.
Figure 1. Bellingham district nurse leg ulcer pathway.
The service development project was evaluated against four measurable objectives:
- To improve the assessment and monitoring of wounds in the community setting, with a specific focus on leg ulcers
- To initiate the collection of local data on the treatment and wound healing progression
- To measure the costs of a new evidence-based treatment on local formulary budget
- To standardise practice and promote continuity of care for patients with a wound treated within the community locality.
The rationale for this intervention was that incorporating an evidence-based intervention in wound treatment would lead to a more consistent approach to wound care in the locality, resulting in improved patient and economic outcomes.
Methods
The district nursing team involved provides care to patients across three GP practices and encompasses a population of approximately 8241 residents. Approximately 21% of the population are older than 65 years, and 18% of residents consider their health to be fair to very poor (Northumberland Census, 2011).
The pathway was developed by the tissue viability team and adapted locally to include named products in collaboration with the district nursing team to identify appropriate wounds eligible for treatment with the UrgoStart treatment range. A Wound Outcome Tracker (WOT), developed and supported by Urgo Medical, was initiated to monitor and track the progression of wound healing. This tool enabled the nurses to understand any advancements in the wound healing trajectory and evaluate the pathway on patient outcomes in clinical practice. The WOT was completed by the nurses at each patient visit (until healing was achieved or the patient was lost to follow-up). Patients were deemed to have been lost to follow-up if they moved out of the area, were admitted to hospital during the implementation period or died. The impact on the monthly dressing expenditure against the allocated budget was monitored using data from the online ordering system by both the nursing and tissue viability teams, to understand any potential economic consequences of the intervention.
As part of the implementation, a project lead from the district nursing team facilitated data collection, coordination and identification of suitable patients included in the treatment and subsequent data analysis.
Urgo Medical supported a training and education programme, which included an update on wound assessment, mode of action and appropriate use of the UrgoStart treatment range. The use of the WOT to further support the data entry was introduced following this initial training.
Findings and results
Clinical outcomes
During the implementation of the pathway including UrgoStart Plus treatment, the WOT was initiated so that information on the wound type and progression could be captured. Over a period of 12 months, holistic assessment was conducted for 24 patients with 33 wounds (Table 1), and these cases were deemed suitable for UrgoStart Plus treatment. Information was not captured for every patient admitted to the caseload with a wound who entered the pathway. However, the information captured indicates the positive results experienced by the sample group, which subsequently reduced the monthly wound care expenditure (Figures 3 and 4).
Table 1. Patients deemed suitable for treatment with UrgoStart Plus over the 12-month study period
| Wound type | Number of patients | Number of wounds | Comments |
|---|---|---|---|
| Venous leg ulcers | 14 | 17 | - |
| Mixed-aetiology leg ulcers | 1 | 4 | One patient had four ulcers; two healed in 2 weeks and the other two in 6 weeks |
| Category 3 pressure ulcer | 1 | 1 | Lost to follow-up |
| Post-operative wounds | 4 | 7 | One patient had four wounds; three patients had one wound each |
| Skin tear | 1 | 1 | - |
| Stoma reversal | 1 | 1 | - |
| Trauma wound | 1 | 1 | - |
| Diabetic foot ulcer | 1 | 1 | - |
| Total | 24 | 33 | - |
 Figure 2. Progression of a leg ulcer over 7 weeks of treatment with UrgoStart Plus. (a) At presentation; UrgoClean Ag initiated with UrgoKTwo (40 mmHg). (b) Week 3; UrgoStart Plus Pad initiated with UrgoKTwo. (c) Week 7; healed, hosiery maintained.
Figure 2. Progression of a leg ulcer over 7 weeks of treatment with UrgoStart Plus. (a) At presentation; UrgoClean Ag initiated with UrgoKTwo (40 mmHg). (b) Week 3; UrgoStart Plus Pad initiated with UrgoKTwo. (c) Week 7; healed, hosiery maintained. 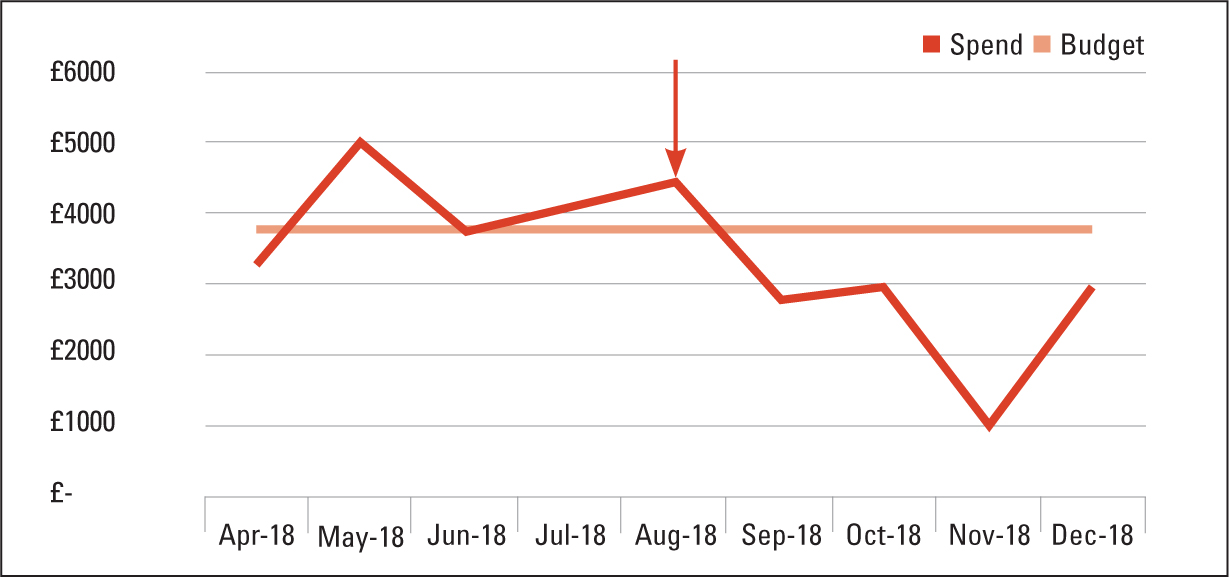 Figure 3. Introduction of UrgoStart Plus treatment
Figure 3. Introduction of UrgoStart Plus treatment 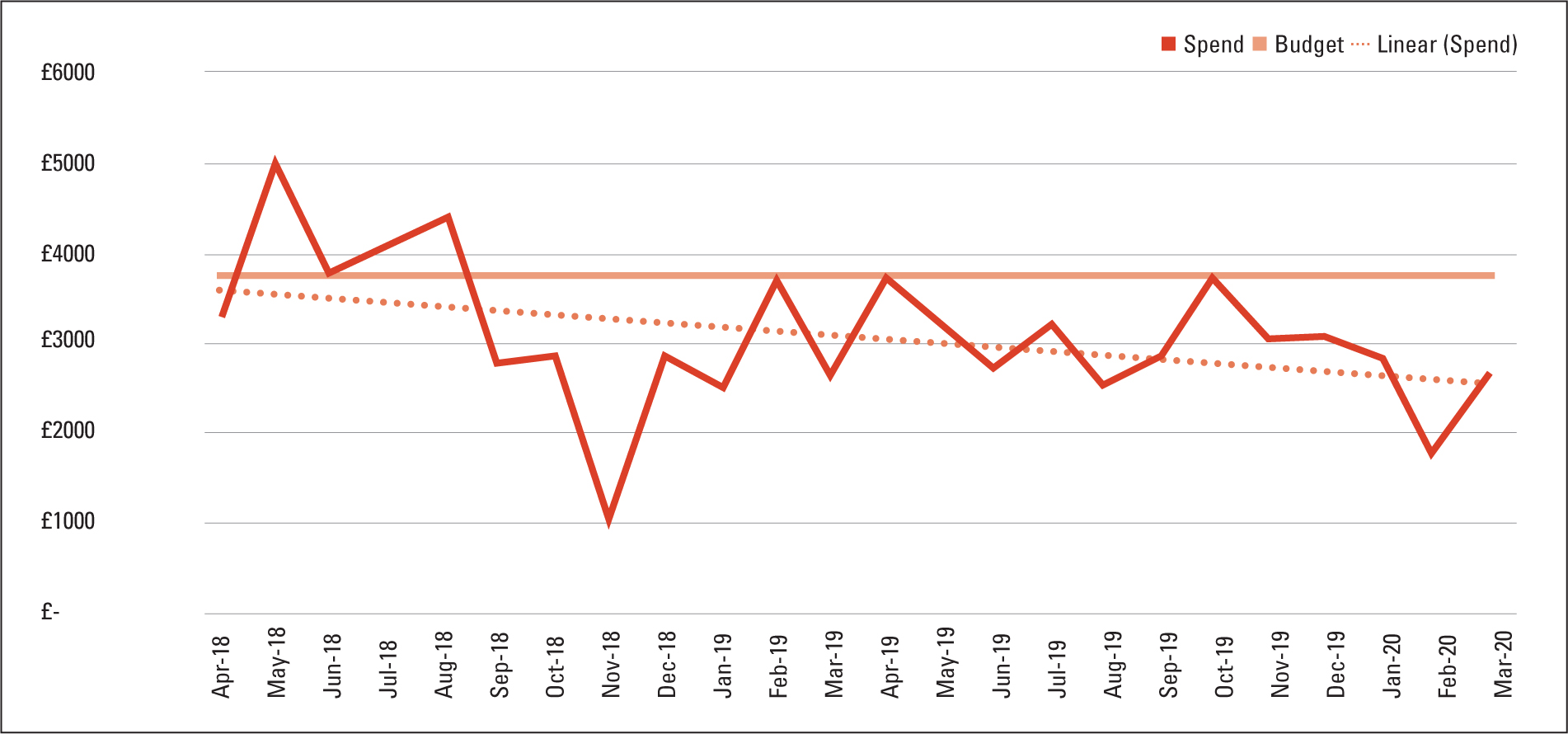 Figure 4. Introduction of UrgoStart Plus treatment and overspend period 2018−2019
Figure 4. Introduction of UrgoStart Plus treatment and overspend period 2018−2019
In relation to VLUs and MLUs, the healing times ranged from 2 to 26 weeks. However, overall, 90.5% (n=19) of leg ulcers healed within 10 weeks. One indolent wound of 104 weeks' duration healed in 16 weeks, and another healed in 26 weeks. Both of these patients had underlying comorbidities, such as diabetes and obesity. The healing times for other types of wounds ranged from 2 to 12 weeks, with an average of 7.2 weeks.
Example case study
A 76-year-old man with type 2 diabetes who had required daily dialysis for the past 3 years was one of those patients deemed suitable for treatment with UrgoStart Plus. He presented with a leg ulcer wound after 3 weeks of ‘self-care’. Figure 2 shows the progression of this patient's wound over the 7-week healing period.
Financial outcomes
Pre-implementation data are available for the 4 months prior to the launch of the UrgoStart Plus treatment, which demonstrated a consistent overspend when compared with the monthly budget.
While the implementation month is also associated with an increased overspend, the 3 months post-launch highlighted a consistent underspend when compared with the budget. Surprisingly, although these months also typically correlate with the start of winter pressures and a period of heightened demand, the spend remained consistently below budget.
When reviewing the 2-year run rate of spend against budget, it was evident that the reduction in overall expenditure was sustained. This included the overspend period April to August 2018 and the corresponding period of April to August 2019.
The UrgoStart Plus treatment introduced in the 2018–19 financial year resulted in an underspend against budget of -£6516 (corresponding to an underspend of 14%), while the full in year effect on the 2019–20 budget was an underspend of -£9967 (corresponding to an underspend of 22%).
Qualitative patient and staff feedback
Qualitative feedback from both patients and staff validated the clinical and economic findings, with many reporting improvements in wound healing following implementation of the pathway. Prior to the introduction of the UrgoStart Plus treatment range, some staff had voiced dissatisfaction with the healing time and the increasing number of dressing changes required to manage patients' wounds. Frustrations with the lack of progress of wound healing had affected concordance, and staff disengagement was evident. Anecdotal evidence was observed of enhanced wound closure, reduced wound size and a reduction in dressing change frequency, following the introduction of UrgoStart Plus, and this resulted in a new willingness to drive changes in clinical practice, together with improved confidence from staff and patients that complete wound closure could be achieved. As a result, concordance with treatment increased. Patient engagement was also enhanced, as the WOT provided a visual demonstration of patients' positive progression through the healing trajectory. Anecdotally, the implementation of this project also appeared to have a positive influence on the patients-reported QoL.
Below are some quotes from the leg ulcer cohort:
‘When you said I had a leg ulcer, I thought I was going to have it for the rest of my life, but you have helped me so much, and I never dreamed it would have healed so quick.’
‘The plasters the nurses use is like magic.’
From the nurses' perspective, the reduction in average wound healing time and dressings spend also contributed towards increased job satisfaction, staff confidence in product administration and enhanced team working. As this was attributable to using UrgoStart Plus and noticeable clinical improvements, the product was expanded for use on all wounds.
‘We want the best for our patients and, with the help of these dressings, the best is what we can provide.’
‘Being a nurse, there is nothing better than healing wounds.’ (community nurse)
‘We are now celebrating good practice.’
‘As a team, we are proud to have healed this patient in a timely fashion, allowing her to go back to work earlier than she first expected. We believe we have saved money and resources using these products. We received a lovely thank you care from the patient.’
‘As a team, we have found increased motivation due to the improved healing time, which has given us high team morale.’
The project aimed to evaluate the introduction of an evidence-based wound care pathway for the management of chronic wounds, with an emphasis on leg ulcers. All its four objectives were achieved.
- Objective 1: The project enabled the district nursing team to undertake a standardised scoping exercise of all wounds of patients on their caseload and to ensure that all patients with leg ulcers had been holistically assessed and were receiving a therapeutic level of compression prior to the implementation of UrgoStart as an adjunct to treatment (O'Meara et al, 2012)
- Objective 2: The use of the WOT enabled the nurses to document the pre- and post-implementation wound characteristics and provided an objective tool, detailing progress in terms of wound size, healing time, etc. A reduction in wound volume was found in all patients over the 12-week evaluation period, and the findings concurred with those of Milne and Jones (2018), who used UrgoClean Ag, UrgoClean and UrgoStart Plus sequentially in combination with compression therapy and found a >75% reduction in wound volume in eight patients; wound volume decreased by <40% in seven patients, and complete wound healing was observed in four patients (Milne and Jones, 2018). This was in line with best-practice evidence of what constitutes normal wound healing (Kantor and Margolis, 2000). In the district nursing cohort, all patients progressed on a wound-healing trajectory with progressive reduction in wound area (excluding one patient lost to follow-up). An additional benefit was that the completion of the WOT following each assessment also met the Nursing and Midwifery Council's (NMC) code requirements for good record-keeping and communication, which is integral to promoting safety and continuity of care for patients and clients (NMC, 2018)
- Objective 3: Although there was an initial overspend at the beginning of the implementation period, the 3 months post-launch highlighted a consistent underspend when compared with budget. The UrgoStart Plus treatment introduced in the 2018–19 financial year resulted in an underspend of -14% versus budget, while the full in year effect on the 2019–20 budget was an underspend of -22% versus budget. This was in line with NICE's estimated cost modelling predictions of potential financial savings of £541 per patient when treating VLUs with the UrgoStart treatment range (NICE, 2019b) for the NHS when used instead of a non-interactive dressing (NICE, 2019a)
- Objective 4: The introduction of an evidence-based pathway locally ensured a standardised and consistent approach to wound care, and the use of the WOT tool enabled nurses to identify which wounds were not progressing normally, so that patients could be referred on for specialist advice and additional investigations and advanced therapies could be implemented in a timely manner (Wounds UK, 2019).
Between 2014 and 2018, there was an estimated 20% reduction in the number of district nurses available, which also reflects the reduction in overall community nursing staff (Heath Foundation, 2019). Therefore, there is a need to consider similar projects, which increase efficiency and productivity, but also release time to care in order to meet future demands on the community nursing service (NHS England, 2019).
Conclusion
A structured approach to wound care in the community is necessary in order to implement care, where the outcomes are measurable, into everyday clinical practice (NHS England, 2018a; National Wound Care Strategy Programme, 2021). The importance of getting consistent evidence-based treatment right the first time from day 1 has been highlighted through the NHS Getting It right First-Time programme (NHS, 2020) and Betty's story (NHS England, 2017).
This small-scale project initially focused on the integration of the UrgoStart treatment range into a clinical pathway for the management of leg ulcers. Based on the success of this structured clinical pathway, which combined good wound care practice and evidence-based wound care products, there is the potential for substantial cost savings for all chronic wound care in the community setting, which other community nursing services may wish to explore.
KEY POINTS
- The implementation of evidence-based practice is vital to achieve positive outcomes, for patients, nursing staff and the overall health service
- There is considerable disparity in wound management practices across the UK; because of this, patient outcomes vary considerably
- Wound management accounts for around half of all nursing care delivered in the community
- Given the increase in the number of people in the community with hard-to-heal wounds and the decrease in community nursing staff, it is imperative to ensure resource optimisation, to ensure that costs can be reduced while maintaining high efficacy
CPD REFLECTIVE QUESTIONS
- What challenges do you face at present in delivering wound care in the community?
- How could you use such a leg ulcer pathway to optimise resources at your organisation?
- What steps could you follow to apply this leg ulcer pathway at your organisation/trust?


