A significant component of providing person-centred care is the fostering of an inclusive, culturally sensitive and holistic approach in clinical practice. However, discrepancies and discrimination in healthcare provision remains a pressing issue, and the discipline of wound care is no exception. Underrepresentation of diverse skin tones in medical education, and many providers’ implicit racial bias, drives inequities in wound care, such as disproportionally poor outcomes for Black patients (Johnson et al, 2023). This is highlighted by several US studies that report that pressure ulcers/injuries (PUs/PIs) are more likely to form, are more severe and are less likely to heal after 90 days in Black nursing home residents than in White residents. This, alongside a multiplicity of other contributing factors, is likely worsened by healthcare providers’ failure to recognise skin changes that signal wound development and progression (Johnson et al, 2023).
Change is happening, as indicated by several developments in the literature, including the recent publication of an international consensus document addressing the necessary signs, symptoms and terminology to facilitate high-quality wound care for all skin tones (Dhoonmoon et al, 2023); however, the progress made in research and education does not yet match the realities of clinical practice. It must be noted that, as Dhoonmoon et al (2023) do indeed point out in the aforementioned consensus document, that those commonly deemed an ‘ethnic minority’ in fact make up the ‘global majority’, a collective term for those who are Black, Asian, Brown, dual-heritage and/or indigenous to the global South, who currently represent approximately 80% of the world's population. Indeed, the UK itself is an ethnically diverse society, with data from the national census showing a decrease in the percentage of the population identifying as being from a White ethnic group, from 94% in 1991 to 81.7% in 2021. The next most common high-level ethnic group was ‘Asian, Asian British or Asian Welsh’, accounting for 9.3% (5.5 million) of the overall population of England and Wales (Office for National Statistics, 2022). This means that a wound care practitioner will likely encounter an increasing number of patients with a wider variety of skin tones in their daily practice, which necessitates faster and greater change in the way that research, education and continual professional development is conducted.
Changing the conversation: consideration in how we talk about wound care
A systematic review of diversity in dermatologic randomised control trials showed that, while racial and ethnic data reporting is becoming increasingly transparent, inclusive representation remains stagnant (Johnson et al, 2023). Indeed, a literature search conducted in 2021 revealed that classroom learning was found to be predominantly framed through a White lens, with White normativity strongly reinforced through teaching and learning activities (Oozageer Gunowa, 2022). This reinforcement of White normativity was evidenced through two main themes:
- Dominance of whiteness in the teaching and learning of PUs in undergraduate nurse education
- The impact and implications for student nurses of whiteness as the norm in PU teaching (Oozageer Gunowa, 2022).
To counter this, in wound care education, there is a need for use of case studies and photographs of dark skin tones to contribute to the knowledge base across the full range of skin tones and to address the bias towards lighter skin tones (Dhoonmoon et al, 2023). Currently, less than 5% of images in medical literature include dark skin tones, which is only slightly higher in dermatological texts (4–18%) (Johnson et al, 2023).
Similarly, the continued use of terminologies such as ‘redness’ and ‘non-blanching skin’ as the only clinical indicators of early signs of pressure damage create a level of disparity in risk assessment for patients with darker skin tones (Dowley, 2023). For instance, ‘erythema’ refers to changes in skin colour caused by increased bloodflow, the detection of which is often used to distinguish infected or abnormal skin areas and which is commonly referred to as ‘redness’. However, erythema does not appear as redness in many skin tones (Dhoonmoon et al, 2023). Instead, changes in colour can manifest anywhere on the spectrum of pink, red and purple; in some cases, it may be limited to a subtle darkening of the existing skin tone (Dhoonmoon et al, 2023). Notably, the frequency of erythema has been found to decrease proportionally with an increasing Fitzpatrick Skin Phototype Classification score, which is associated with skin tones with a high amount of pigment (Johnson et al, 2023). This is only one of the many ways in which inappropriate widespread application of Eurocentric language can actively harm patients.
Changing practice: practical steps towards equality in care provision
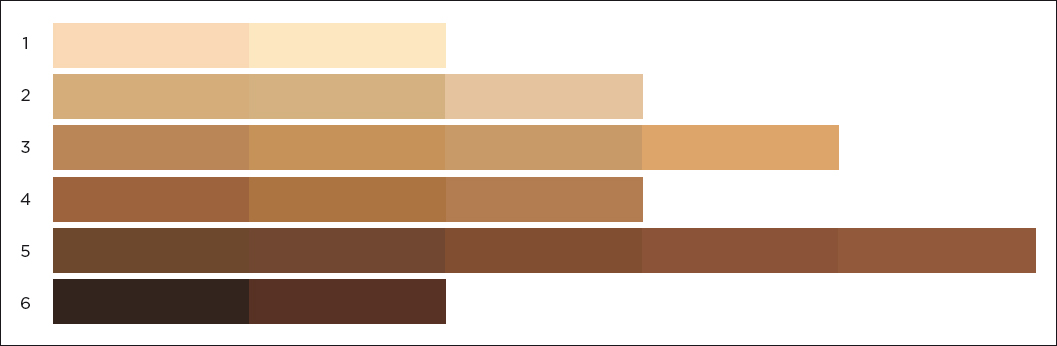
Patient assessment is the foundation of all care, and a truly person-centred wound assessment is holistic and inclusive, taking into consideration a patient's health; environment; physical, psychological and psychosocial factors; and elements related to their ethnicity, including their skin tone. The skin tone tool (adapted from Ho and Robinson, 2015) is a validated classification tool that shows a range of skin tones, so that the tone which most closely matches the patient's inside upper arm can be selected to establish a baseline (Dhoonmoon et al, 2023). This baseline will aid in diagnosis by making any skin changes easily identifiable. Relatedly, it will also reduce the likelihood of the attribution of these alterations to a sinister underlying cause, when they might instead be due to age-related hyperpigmentation; comparing the affected area to another part of the patient's body may be helpful in this regard (Dhoonmoon et al, 2023).
Similarly, as there is often less of a visual evidence base for assessment and diagnosis in patients with darker skin, it is important not to rely solely on appearance to assess a patient's skin, in case visual signs are missed. Indeed, in a post-hoc analysis of 350 chronic wounds from a prospective 14-site clinical trial, Johnson et al (2023) found that, despite equivalent wound bacterial loads, clinicians detected erythema, delayed wound healing and wound breakdown and enlargement less frequently in patients with high skin pigmentation. To counter this, full use of the senses—particularly touch—is valuable, with changes in texture and temperature being the key indicators of pathology: affected skin may feel tighter or more swollen (oedema), indurated (hardened or lumpy), warmer (inflammation) or cooler (tissue hypoxia) in comparison to other areas (Dhoonmoon, 2023; Dowley, 2023). A loss (as well as a deepening) of pigmentation may be indicative of pathology, as white or grey discoloration may imply tissue damage (Dowley, 2023).
Conclusions
Only conscious effort over time will reduce the inequalities in healthcare systems. Recent developments in the literature represent a positive change, but these must be reinforced by the adoption and development of different approaches to wound care in education, research and practice.