NHS community services are an essential part of the national effort to support people to manage their conditions, prevent ill health and deliver care closer to home. Community nurses are central to the care delivered for many people across a broad range of conditions and needs. If further proof were needed of their importance, the response to COVID-19 has been underpinned by a robust offering by the community sector, allowing earlier discharge from acute settings and managing a range of complex conditions that would previously only been managed within a hospital. Community staff and community nurses have risen to the challenge and demonstrated their value.
On an anecdotal level, we know this to be true, but this does not support business cases. A feeling that community nursing is important does not allow investment to be committed to the service. How do we quantify the difference that a community nurse makes? How do we demonstrate the economic value of community nursing?
These were the questions addressed at a roundtable hosted by the Healthcare Financial Management Association (HFMA) in 2021, attended by a mixed group of directors of nursing, directors of finance and subject matter experts.
Why does the economic value of community nursing matter?
The most recent national cost collection data showed that, in 2019/20, community nurses across England (district nurses, specialist nurses and school nurses), working in NHS organisations, had 42.4 million contacts at a cost of over £2 billion (NHS England, 2020).
It is important to note that cost data is only submitted by NHS organisations, and we know that a significant number of community services contracts are held by non-NHS bodies, such as social enterprises. Therefore, the actual number of contacts is likely to be considerably more. The numbers show that community nursing represents a significant part of healthcare delivery in England.
However, community nursing struggles to demonstrate its value to system partners. A NHS Benchmarking report (NHS Benchmarking Network, 2019) found that investment in district nursing had fallen by 2.6% from 2013 levels. Anecdotally, it is well known that the service supports people to stay at home and avoid hospital admissions. Community nurses support discharge, signpost people to other services that can help support them and are key to integrating care around a patient—the building blocks for all effective integrated care systems (ICSs). However, because the breadth of the service is so vast and some of the benefits can be difficult to measure, when compared with discrete hospital interventions such as a hip replacement, demonstrating the economic value is difficult. This means that it can be a challenge to secure investment in the service.
With constrained financial resources, organisations and systems need to be able to demonstrate the impact that any investment will have. If a service cannot be quantified, there is little space for a leap of faith that it is the right thing to do. Indeed, the stability of district nursing as a core part of the NHS' offer may even work against it. It can be seen as a comfortable and reliable service, something that is always there, and not innovative or dynamic—a necessary service to care for people. This could not be further from the truth, but community nursing, as a profession, needs to show how integral it is to system working.
Truly integrated care starts by putting the patient at the centre of their care and decision-making, organising services around the person. This has formed the basis of the government's most recent white paper (Department of Health and Social Care, 2022), which considers how to deliver more joined-up care for people. For community nursing, this presents an opportunity to raise the profile of the service and demonstrate how fundamental it is to the delivery of integrated care, benefiting both patients and the health and care system.
Community nursing is one part of a wider multi-disciplinary approach, which is likely to expand as ICSs become established. To ensure that the community nursing voice is heard among the many demands for resources, value needs to be demonstrated going forward, not as a retrospective analysis of ways of working that may no longer be as relevant.
What do we mean by economic value?
Any conversation about ‘value’ must start from the patient perspective: what are the outcomes that matter to a person? Value in health care has largely been based on the work of Professor Robert Kaplan and Professor Michael Porter of Harvard Business School in the US, who define value as the ‘health outcomes achieved that matter to patients relative to the cost of achieving those outcomes’ (Harvard Business School, 2022), putting the patient centre stage. This is often referred to as technical value (Box 1).
Box 1.Case study: improving technical valueOne roundtable participant's trust has introduced a new pathway for patients with leg ulcers. Previously, patients would have their leg ulcers treated on a regular basis for many years. The new pathway, involving a different intervention carried out by a specialist leg ulcer nurse, has shown a 12-week healing rate. Not only has the outcome for patients improved, but also the level of resources required has reduced.
For those commissioning services, allocative value (or population value) has to be considered—how should healthcare resources be allocated across a system to maximise outcomes for the local population?
The NHS needs to consider allocative value alongside technical value. A hospital might optimise its treatment pathway so that admitted patients receive the best possible care in that setting. However, this is only part of the patient's pathway; real value might be delivered if the patient had not been admitted in the first place. If someone had been identified earlier as needing support, with that support being provided in a community setting, it may well have delivered better outcomes for patients by avoiding a hospital admission and—at a system level—reduced overall costs of treatment.
The impact that community nursing can have on allocative efficiency should not be underestimated. Specialist community nurses enable capacity to be freed up in acute trusts, which not only reduces waiting list delays, but indirectly reduces the chances of someone's condition worsening while they are waiting for treatment.
Personal value means improving the outcomes that matter to an individual for a given amount of resources used—not only by the health system, but also by the individual and their family, recognising that the experience of care is a critical element.
A fourth measure of value is social value (Box 2). Delivering services in the home is not only beneficial for the person and the NHS. By spending less time in hospital, the impact on day-to-day life is dramatically reduced. This has an effect on the patient's ability to undertake and remain in employment; it can also support children and families to access education more consistently, with the person maintaining their community links, which may support others. There is a significant benefit to society, created by community nursing and wider community-based services. Stable employment is a major factor in maintaining good mental health, and the NHS Long Term Plan (NHS, 2019) identifies this as one of several wider social goals that it seeks to support.
Box 2.Case study: hospital at home serviceThe hospital at home service in Sussex looks after ‘sub-acute’ patients, who would normally remain in a hospital bed but can be supported in their own homes.The service is commissioned from Sussex Community NHS Foundation Trust by the acute provider, Brighton and Sussex University Hospitals NHS Trust. Patients remain under the care of an acute consultant while being cared for in their own homes, but the service is delivered by community nursing staff.Currently the service covers:
- Anti-microbial therapy pathway
- Bronchiectasis admission avoidance pathway
- Negative pressure wound therapy for vascular patients.
Other pathways are in development as the service expands.For the patients, this service allows them to get on with life; some still work or continue their own caring responsibilities while having treatment. Staff have noticed that patients tend to recover faster in their own home, both physically and emotionally, and the readmission rate is very low.The service receives positive feedback from the patients. An example is shared below:‘The outstanding service allowed me to avoid hospital admission and receive treatment at home. I have two young children (3 years and 18 months) and was able to continue being their main carer. The team came to my home three times a day to administer intravenous antibiotics and were always flexible to fit around any family commitments. They were utterly brilliant with my children and helped to keep them entertained while I was immobile.’Financial analysis has shown a saving of 27% when compared with the same treatment at the acute trust. The service has released bed capacity and has helped to better manage demand (HFMA, 2019).
The challenges of measuring value
In order to measure value, a number of data building blocks are required, as set out below:
- Method of categorising patients: grouping patients with similar needs or characteristics
- Interventions: non-pharmacological and pharmacological (eg wound care and drugs prescribed)
- Outcome measures: the change in health attributable to an individual or series of interventions
- Use of resources: the resources consumed during the intervention (eg staff time, medicines, etc). The currency for measuring the amount of resources used is usually cost, but could be something more meaningful to clinicians (eg the number of hours a community nurse spent caring for a patient).
The HFMA's Healthcare Costing for Value Institute works with the NHS to develop effective approaches for measuring value.
Recording data
Understanding the activities undertaken in community services has been an ongoing challenge for the sector. The development of the national community services dataset (CSDS) is one of several steps being taken to better understand community activity. Data is submitted by both NHS and non-NHS providers of community services; non-NHS providers are believed to hold around half of all publicly funded community services' contracts.
National data can only be robust if it is supported by good local data collection. The roundtable participants highlighted that this continues to be a challenge and that there is a need for cultural change within community nursing to facilitate good data collection. The use of mobile technology to record patient contacts appears to be uncomfortable for many, with stories of staff regularly returning to the office to fill in the associated paperwork.
Community nurses need to be easily able to record information during a care contact, whether that be face-to-face or by telephone. The IT system also needs to support the business needs of the organisation; the data entered by community nurses should be sufficient in quality and completeness to both support clinical care and directly feed the necessary organisational reports without the need to request further information.
This difficulty in collecting organisational data illustrates that the importance of demonstrating value is not just about securing investment from commissioners. Community nurses themselves need to understand the importance of measuring value and of being able to evidence the difference that they make to people's lives. Cultural change is essential, and it needs to be driven from within the service.
Data quality
Even where activity data is routinely collected, the quality of it may not be sufficient to enable analysis. This could be due to confusion on how to classify a contact, or may be linked to the way that the IT system is structured. Many IT systems are adaptations of those created for use in acute settings and do not fully represent the nuances of community nursing provision.
Measuring outcomes
Outcome data is a key building block when measuring value. Although the NHS collects a significant amount of clinical data, many of the measures focus on processes or outputs, rather than outcomes.
Community nursing outcomes are often described as the absence of things: admissions avoided, bed days saved, and so on. These are valuable outcomes for a commissioner focusing on the demand issues at an acute trust, but they do not recognise the other positive outcomes that community nursing can support. Outcomes must also be defined by working with patients and the wider community. To deliver value is to deliver the best possible outcomes for the patient, and it is important to understand what those are.
Understanding activity
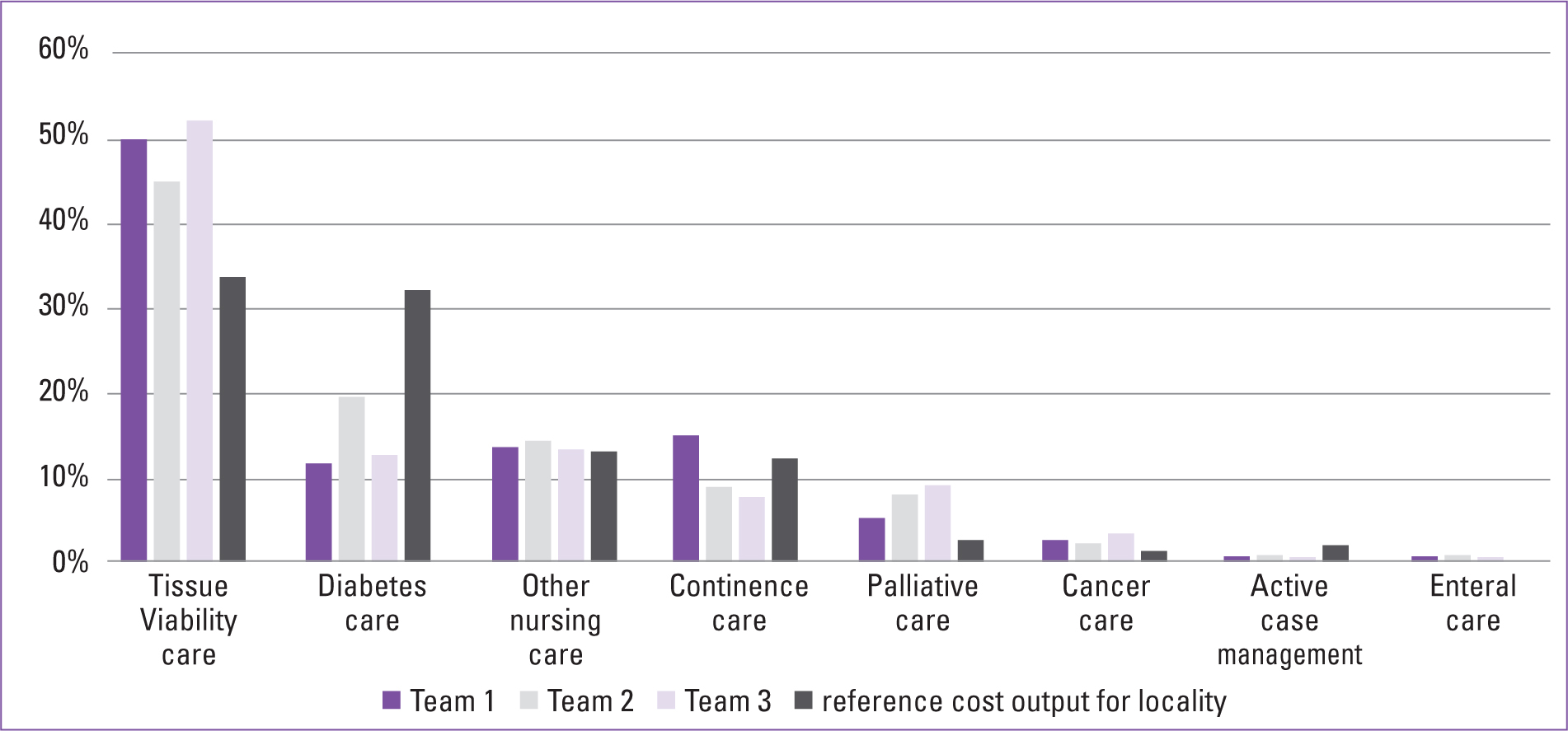
Measuring the value of community nursing activity requires a method of categorising patients with similar needs or characteristics so that benchmarking can be undertaken. It is widely recognised that the current method of measuring community nursing activity (by number of contacts) does not provide the level of information required for comparing services. See Box 3 and Figure 1 for an alternative method of data collection.
Box 3.Case study: Improving intervention information for community nursing servicesTypically, the recording of clinical activity for NHS community services has been very limited, with national datasets only collecting contact data for face-to-face or non-face-to-face interventions, and one or multiple patient contacts with one clinician. Gloucestershire Health and Care NHS Foundation Trust has developed its clinical system so that more detailed information about the delivery of district nursing services can be collected.One development has been a change in approach to the collection and recording of interventions provided to patients on district nursing caseloads, with a subsequent improvement in the accuracy of the grouping of activity into healthcare resource groups (HRGs).Previously, all interventions were recorded by district nurses, with a decision being taken later by senior clinical staff as to what was the most significant intervention. This would then drive the allocation of the most suitable HRG code. A pilot programme now provides the ability for each nurse to identify the primary intervention within each contact or episode so that the most appropriate HRG will be generated. The accuracy of information collected has been improved by clinicians using mobile devices when they are with patients. Figure 1 shows how these data improvements provide a clearer picture of the needs of the caseloads in three locality teams, and highlights the high proportion of tissue viability and palliative care interventions compared with the expected percentage calculated using previous reference cost data (HFMA, 2021).
Applying costs
Ultimately, the demonstration of value will need to be translated into financial terms, where it is to be used to secure ongoing or additional investment into community nursing. Good costing data underpins the assessment of value and informs the allocative efficiency of systems.
Those at the roundtable emphasised that the first step to understanding value is to get the activity data right; however, this must be followed by the application of costs. From a national perspective, the two are being developed simultaneously, with the mandating of the collection of patient-level cost (PLICS) data in community services from 2021/22.
Conclusion
The remit of community nursing is vast, and this presents a problem when trying to demonstrate value, which requires definition of activities and outcomes. Community nursing creates value under all definitions of the term, and it is essential that this is quantified so that the profession is recognised for its essential role within the NHS and in wider society. Measuring value is not just about securing investment in services, although this is welcome. It is about demonstrating the role that community nurses play in supporting people to stay well, manage conditions and remain in their communities. It is about explaining how community nurses support other services within a system, through integrating care around a patient and avoiding unnecessary interventions.
With the increasing focus on system working and health and care integration, community nursing services have an opportunity to demonstrate their value and their pivotal role in the future of the NHS. Demonstrating value will always be difficult, and obtaining the data will remain challenging until it becomes routine. Therefore, we must make a start on measuring the economic value of community nursing, to instigate the change that is needed.
The full report can be found at: www.hfma.org.uk/publications/details/measuring-the-economic-value-of-community-nursing.
Key points
- Community nursing represents a significant part of healthcare delivery, with an annual spend of over £2 billion on district nurses, specialist nurses and school nurses. Community nurses deliver care in a wide range of locations in many different types of organisations. The plethora of provision and activity can make it hard to articulate the value of their role.
- Integrating care at a patient level is fundamental to an effective integrated care system (ICS). Community nurses have a key role to play in supporting the success of the ICS structure. Any assessment of the economic value of community nursing must be forward thinking.
- The completeness and quality of activity data are huge issues for community services, with some services still using paper records. Historically, the level of investment in informatic infrastructure in community services has tended to be low, as income has not been dependent on the quality of the recorded quantity of healthcare outputs. Until data quality improves substantially, it may be hard to measure the economic value of community nursing. Improving the quality of data not only requires leadership and investment; it also demands cultural change. Community nurses need to understand the importance of recording good data to evidence the impact they have on people's lives.
- The triple value model (personal, technical and allocative value) provides a useful framework when assessing the economic value of community nursing. The contribution community nursing makes to social value and tackling health inequalities also needs to be measured. A more comprehensive standardised approach to the collection of outcomes measures is required. As well as looking at clinical outcomes, it is important to measure value in terms of outcomes that matter to patients.
CPD reflective questions
- What are the main challenges of articulating the value of the community nursing role?
- What is the contribution of community nursing within the new integrated care system (ICS) and place-based landscape?
- How can community nurses ensure that they record good data to evidence the impact they have on people's lives?

