In various nutritionally vulnerable patients where oral food intake is compromised or completely unachievable, enteral tube feeding is an essential method of nutritional support, involving the administration of liquid feeds via feeding tubes, which is frequently used in hospital and community settings (Scott and Bowling, 2015). Adult patients include those who experience dysphagia secondary to their condition, such as those who have had a stroke, and those that have ongoing neurological diseases, profound learning disabilities, and cancer treatments; for example, head and neck or gastrointestinal cancers (Stratton et al, 2018). For some patients, enteral tube feeding is a short-term intervention used during post-operative care or intensive care treatment; however, the number of patients receiving long-term or permanent enteral tube feeding is increasing, with many independently managing this in their own homes or with support in care homes (Ojo, 2015).
Enteral nutrition can be delivered using a variety of feeding routes and tubes. The use of fine-bore nasogastric tubes (NGT) is a well-accepted method of delivering enteral nutrition; however, it is not appropriate for all patients and is not indicated for use longer than 4–6 weeks (Gkolfakis et al, 2021; Bischoff et al, 2022). Passing an NGT requires the patient to perform, to some degree, a swallowing action, ruling out those with severe dysphagia (Sigmon and An, 2022). Likewise, patients with malignant tumours obstructing the throat or oesophagus are at high risk for NGT placement (Malik, 2020). To overcome such challenges, gastrostomy tubes were introduced in the 20th century. Initially inserted surgically, the practice progressed to less invasive insertion techniques with the introduction of percutaneous endoscopic gastrostomy (PEG) tubes and radiologically inserted balloon retained gastrostomy tubes (RIG) tubes (Welbank and Kurien, 2021).
PEG tubes are passed through the oesophagus using an endoscope and anchored in situ with a permanent internal bumper—a disc wider than the stoma incision—which sits flush against the internal stomach wall. Externally, the tube has a fixation device that should sit approximately 2–5 mm from the skin surface (National Nurses Nutrition Group (NNNG), 2013) and can be opened and repositioned to allow for skin hygiene and general routine care. A standard PEG tube can remain in situ for several years but may eventually become less viable and require a planned replacement (Gkolfakis et al, 2021). When replacement is needed, patients can undergo further endoscopic or radiological interventions that facilitate a like-for-like PEG tube replacement or have a balloon gastrostomy tube (BGT) inserted following planned removal of the existing PEG. The latter is less invasive and, for some patients, is the only option if endoscopic placement is not possible (Best, 2019).
The term RIG describes how these feeding tubes are placed using X-ray to guide tube insertion (Rajan et al, 2022); in this instance, a BGT is used as the first line. RIGs are preferred when the oesophagus is too narrow to safely pass an endoscope, for example, in some gastro-oesophageal cancers (Bossola et al, 2022). The tube is initially held in situ with removable sutures or gastropexies, securing the external fixation device to the abdominal wall. Internally, BGTs are held in position by a silicon balloon inflated with water (~5 mls), which acts as the internal bumper. Post-insertion, this balloon water requires relatively regular removal and replacement, to ensure the water is not absorbed over time through osmosis, leaving the tube at risk of displacement (Baskin, 2006; National Institute for Health and Care Excellence, 2006; Shah et al, 2018). Regular checks also allow for the monitoring of leakages and balloon-related concerns. In addition to routine balloon water changes, the entire BGT requires routine replacement to reduce the rates of emergency care needed for damaged and displaced tubes (Cominardi et al, 2020). There is a lack of clear guidance on when to perform the first BGT replacement post-initial insertion; however, it is generally performed between 3–8 months, after the stoma tract has fully healed (Shah et al, 2018; Cha et al, 2022). Routine replacements are thereafter carried out every 3–9 months, depending on individual patient requirements or manufacturer guidelines (Best, 2019).
Patients who are more active and find the BGT too bulky and uncomfortable, or those who are likely to pull at their tube, increasing the risk of a traumatic displacement, may be offered the choice of a low-profile device (LPD), otherwise known as a button (Al-Balas et al, 2023). The LPD external fixation device sits on the abdominal skin surface without a permanent length of tube attached to it. It is anchored in position with a balloon inflated with water; like the BGT, this water requires regular checks and replacement. As with a BGT, an LPD will require routine replacement of the entire device, usually performed every 3-6 months; however, this may differ for some patient groups or due to different manufacturer guidelines. Following each BGT/LPD replacement, the healthcare professional (HCP) carrying out the procedure must obtain a sample of gastric aspirate to confirm that the tube is positioned inside the stomach and not within the abdominal cavity (NNNG, 2016). Data suggests there are ~23 000 adult patients in the UK who are receiving home enteral feeding (HEF), with ~3000–3500 reported new annual registrations (Stratton et al, 2018). In this patient population, enteral tube feeding can be used as a sole source of nutrition or supplementary to oral intake to meet the entire or partial nutritional requirements (Stratton and Elia, 2007; Gandy, 2014).
Homecare services were first introduced in the UK and elsewhere in the 1990s, and generally include the delivery of enteral feeds, ancillaries and feeding pumps, and the provision of specialist community homecare nurses (CHN) to support patients in managing HEF independently. CHNs can deliver all aspects of education and clinical support for HEF patients in the UK, in partnership with their managing HCP. This can include visiting new patients, their families and caregivers in the hospital setting, before the patient is discharged home to provide training and information about tubes, feeding methods and techniques, including medication administration, if required. Depending on local arrangements, CHNs can provide routine follow-up care in the community, including routine and emergency tube replacements, provided the tube had not been traumatically displaced, and management of unplanned care needs relating to HEF, such as tube repairs or clinical assessments of stoma site complications.
Routine planned BGT/LPD replacements are often performed within the patient's home by a trained professional, such as a CHN or other specially trained community HCP. BGTs and LPDs risk tube displacement if the balloon water is not regularly monitored or cared for effectively, or if the balloon bursts (Gkolfakis et al, 2021). Occasionally, tubes are advertently or inadvertently forcefully tugged, resulting in the permanent internal bumper, or inflated water-filled balloon, being pulled out via the stoma; this is termed traumatic displacement. Such displacements can potentially cause trauma to the internal layers of the abdominal wall, including the peritoneum, which in severe cases can result in life-threatening peritonitis (Cmorej et al, 2019) and have significant cost implications. Any unplanned displacement of a gastrostomy tube necessitates an urgent replacement as the stoma can quickly begin to close and, in some cases, completely heal (Cmorej et al, 2019). Urgent assistance is required to prevent stoma closure, which can occur in 1–2 hours, resulting in the patient requiring hospital attendance to re-site the stoma and replace the gastrostomy tube (Shah et al, 2018). This is undesirable both from a patient care and health economic perspective. Evidence demonstrates that patients who receive home care have lower depression and anxiety scores than those treated in hospital, thus enhancing the care experience and quality of life for an often vulnerable population of patients (Arsenault-Lapierre et al, 2021).
Furthermore, patients are unable to receive their daily nutrition via the feeding tube and may, therefore, be at risk of malnutrition if left without a feeding tube for a long period. If appropriate, patients are provided with specific training by the CHNs, or other trained HCPs, on how and when to insert a stoma preservation device (SPD) to maintain patency of the tract until a new tube can be inserted. The SPD must be inserted as soon as possible to prevent the stoma from healing completely (Cmorej et al, 2019) and allows time for planned hospital attendance, medical review and insertion of a new gastrostomy tube. In cases where the patient cannot insert an SPD, they are usually advised to attend a hospital emergency department for a medical review before receiving a replacement gastrostomy tube in hospital.
The COVID-19 pandemic created a pressing need to avoid unnecessary hospital admissions. It had an enormous negative impact on UK NHS resources and healthcare workers (NHS England, 2021a), including disruptions to planned surgeries and oncology care (Swainston et al, 2020). Hospital attendance became a last resort to protect healthcare resources and prevent the spread of COVID-19, particularly to vulnerable groups at high risk of morbidity and mortality associated with COVID-19 infection (Fisher et al, 2021). Many patients receiving HEF were deemed clinically extremely vulnerable and advised to shield at home (Kemp et al, 2020). It was quickly recognised that revised ways of working would be required to prevent hospital admissions. Aspects of care provided by CHNs were reviewed with traumatic displacement of gastrostomy tubes identified as an area where an emergency hospital attendance, and potentially an admission, could be avoided with a CHN-led replacement service. However, published evidence to support the practice of replacing traumatically displaced feeding tubes in the community was lacking. Clinical practice across the UK relied on local policies, leading to inconsistent community support depending on where the patient lived. Therefore, this research aimed to evaluate the implementation of community replacement of traumatically displaced feeding tubes by CHNs, to assess safety and potential cost savings.
Methods
A multidisciplinary team from the homecare provider (Homeward, Nutricia Ltd, UK) and staff from the NHS managing the care of patients receiving HEF was formed to develop a safe and comprehensive service for replacing traumatically displaced feeding tubes supported by a robust set of guidelines, risk assessments, and training. Local areas where existing policies permitted NHS HCPs to replace feeding tubes in the community, and those which did not, were included. However, due to COVID-19, the HCPs who could perform community replacement of feeding tubes had been redeployed to acute services, and support from the homecare provider was therefore required.
Any adult patient (aged ≥18 years) presenting with a traumatically displaced feeding tube across 17 participating UK NHS Trusts was considered for the community tube replacement service. Data were captured for each patient, including age, sex, diagnosis, type of feeding tube in situ, remaining water in BGTs, whether an SPD was in situ, and cause of tube displacement. Experienced, trained CHNs were required to complete a risk assessment for each patient presenting with a traumatically displaced feeding tube, which included a clear decision-making pathway (Figure 1). If any question flagged a serious risk (e.g. abdominal pain), the tube replacement would not proceed, and the patient was referred to acute care or an alternative trained community HCP, if available, for assessment.
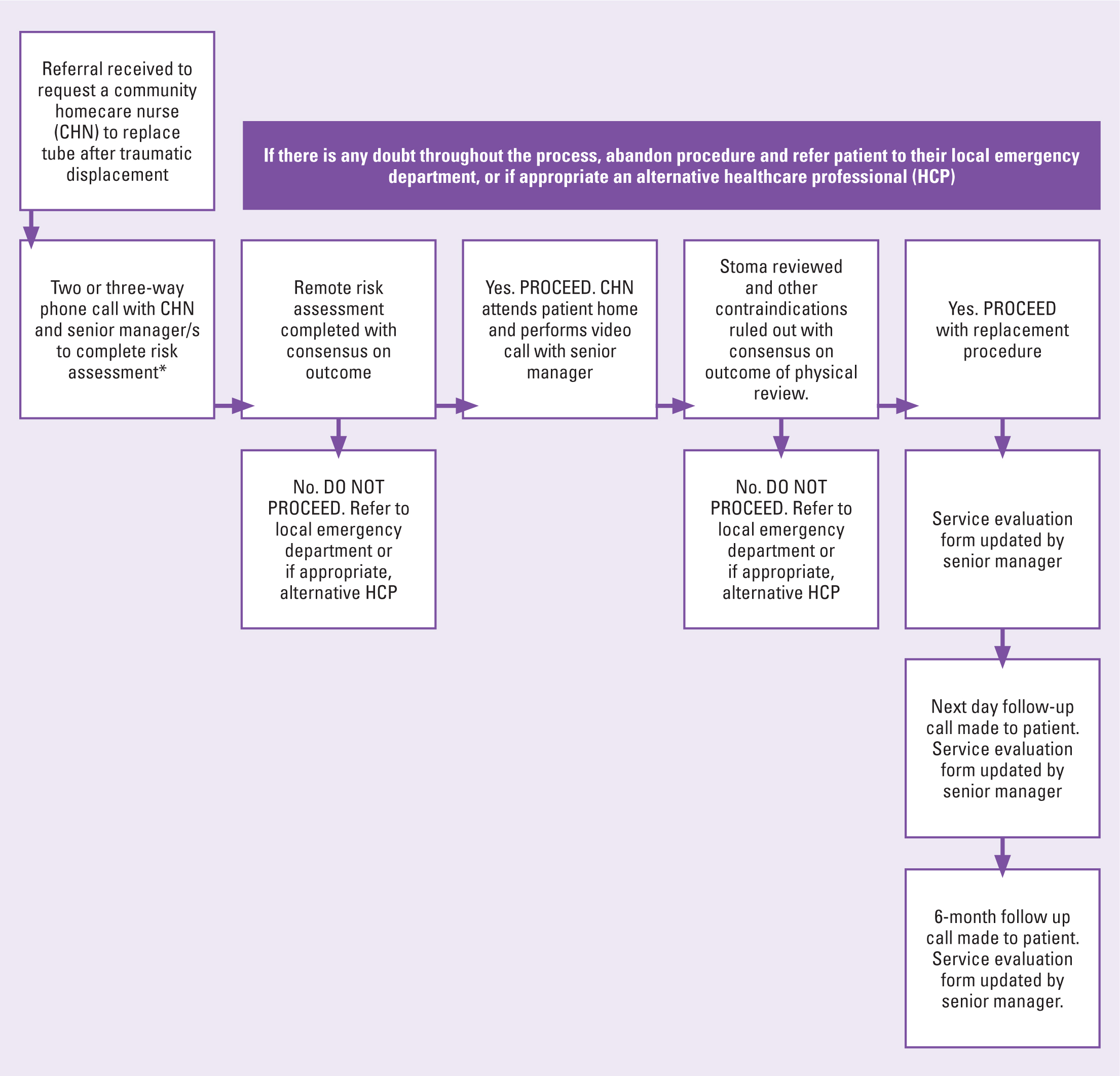
Initially, the CHN was required to perform a three-way telephone call with at least two other senior managers (reduced to one after 6 months), where the risk assessment was discussed, and the outcome agreed by all three individuals. The CHN was supervised by video phone call to ensure there were no visual signs of trauma that would contraindicate the procedure. Where both the risk assessment and physical review suggested it was safe and appropriate to continue, the CHN would replace the feeding tube. If any concerns were raised by the CHN, or senior managers, the procedure would stop immediately, and the patient was referred to acute care for assessment or, in some NHS Trusts, assessed by an alternative community HCP.
Following tube replacement, a gastric aspirate would be obtained to confirm the tube position in the stomach prior to any feeding or flushing, and patients were advised about red flag symptoms to be aware of for 72 hours post-tube replacement (Healey et al, 2010). Red flag symptoms included abdominal pain or discomfort during or after tube use, excessive gastric leakage, or fresh bleeding from the stoma site. If these symptoms developed, the patient was advised to immediately stop using the tube and contact emergency services (Healey et al, 2010).
After each successful tube replacement procedure, a follow-up call was made to the patient/carer the next day to review and ensure there had been no concerns since the tube was replaced. Subsequent follow-up calls were made 7 days post-procedure and at 6 months. At each follow-up intervention, the patient/carer would be reminded of the red flag symptoms (Healey et al, 2010), as an additional safety precaution. During the follow-up period, the senior manager completed a review to ensure all steps had been followed, including follow-up calls and the quality of CHN documentation.
A simple cost analysis was undertaken on a per-patient basis exploring the estimated cost of healthcare resources that would have been used had the patients needed a visit to the emergency department for assessment and management of their displaced feeding tube. Data were analysed based on whether an alternative HCP could have undertaken the tube replacement in the community or not (thereby requiring hospital attendance). Service and treatment costs were obtained from the National Cost Collection for NHS England (2021b). This included the cost of ambulance transport (£390.08), Category 4 emergency department care (£717.78), (Category 4 refers to attendance at A&E departments or urgent care centres such as urgent treatment centres, minor injuries units, and walk-in centres (NHS England 2019)), emergency admission and gastrostomy tube replacement (£4786.00). The total cost for a single patient attendance resulting from a traumatically displaced feeding tube was estimated to be £5895.86. For simplicity, any additional inpatient procedures, other clinical interventions, and costs associated with any social care assessments required to enable safe discharge were excluded (Table 1).
Table 1. Patient demographics
| Patient characteristic | Value |
|---|---|
| Age, years; mean (SD) | 60 (24) |
| Male; n (%) | 31 (52) |
| Female; n (%) | 29 (48) |
| Diagnosis | |
| Learning disabilities; n (%) | 16 (27) |
| Stroke; n (%) | 14 (23) |
| Cerebral palsy; n (%) | 9 (15) |
| Huntington's disease; n (%) | 6 (10) |
| Head and neck cancer; n (%) | 6 (10) |
| Cerebral trauma; n (%) | 5 (8) |
| Multiple sclerosis; n (%) | 4 (7) |
| Tube type | |
| PEG; n (%) | 5 (7) |
| BGT; n (%) | 52 (73) |
| LPD; n (%) | 14 (20) |
Note: Percutaneous endoscopic gastrostomy (PEG); Balloon gastrostomy tube (BGT); Low pro⊠le device (LPD)
Results
A total of 85 requests to replace a gastrostomy tube following traumatic displacement were received between 19 May 2020 and 31 October 2022 from 17 participating NHS Trusts, of which 71 were performed successfully. The remaining 14 were deemed clinically unsafe for tube reinsertion at home and these patients were referred to acute NHS services. Of the 85 requests, 11 patients required more than one tube replacement; therefore, a total of 60 individual patients had at least one tube replacement procedure. Of the 60 patients, 29 were male, and the mean age of the population was 60 years (SD= 24, range: 19–93 years). The most common diagnosis in this patient population was profound learning disabilities (n=16), stroke (n=14), and cerebral palsy (n=9)
Of the 71 tube replacements performed, five were PEG tubes, 52 were BGTs, and 14 were LPDs (Table 1). The remaining balloon water volume was captured for 55 of the 66 displaced BGT and LPD tubes, the mean water remaining was 3.63 ml (SD=1.7, range: 0.2-7ml). The most common cause of tube displacement was confusion (n=11), followed by accidental tube displacement during routine care (n=5), deterioration of the internal bumper (PEG only, n=5), and displacement during/after balloon water change (n=4). There was no reason captured for 29 patients representing 40.8% of tube replacement procedures performed (Table 2). All procedures were carried out within 6 hours of tube displacement, 86% (n=61) had an SPD in situ upon nurse's arrival, and the mean average pH gastric aspirate reading, confirming gastric position post-tube reinsertion, was 2.57 (SD=0.9, range: pH 2–5). Of the 71 tube replacement procedures completed, 31 could potentially have been managed by an alternative local HCP trained to replace gastrostomy tubes in the community; however, for 40 cases, there was no community alternative.
Table 2. Documented reasons for traumatic displacement of gastrostomy tube
| Reason for tube displacement | n | (%) |
|---|---|---|
| Confusion | 11 | (15.4) |
| Accidental displacement during routine care | 5 | (7) |
| Deterioration of internal bumper | 5 | (7) |
| Displaced during/after balloon water change | 4 | (6) |
| Coughing | 1 | (1.4) |
| Body tremors | 1 | (1.4) |
| Caught and pulled by cat or dog | 2 | (2.8) |
| Pulled during changing stoma dressing | 1 | (1.4) |
| Internal balloon water leaking | 1 | (1.4) |
| Unknown reason/not witnessed | 11 | (15.4) |
| Reason not documented | 29 | (40.8) |
All patients received an initial follow-up call on the next working day, within 7 days of the procedure, and at 6 months. During these calls, patients/carers were asked if there had been any pain, discomfort, or any other concerns following the tube replacement, with 100% of patients reporting no clinical issues at any time point.
Some 14 replacement requests were assessed and deemed clinically unsafe to proceed for various reasons, including evidence of bleeding and trauma (n=5) and stoma closure (n=3) (Table 3).
Table 3. Documented reasons as to why a nurse did not proceed with the gastrostomy tube replacement
| Reason not to proceed | n (%) |
|---|---|
| Evidence of bleeding/trauma | 5 (36) |
| Stoma closed, unable to insert a new tube | 3 (24) |
| Tube with capsulated bumper displacement | 1 (7) |
| Tube displaced with overinflated balloon (18 mls) | 1 (7) |
| Withdrawal of patient consent for procedure | 1 (7) |
| Parent replaced tube before nurse arrival | 1 (7) |
| Unknown time of tube displacement, no SPD in situ | 1 (7) |
| 14 fr SPD inserted into a 12 fr stoma tract | 1 (7) |
Note: SPD = stoma preservation device
Potential cost implications were calculated on a per-patient basis, estimating the total cost for a single patient hospital attendance to be £5895.86. The cost of all patients (n=40) without a potential alternative community HCP, who would have accessed emergency services, totalled an estimated £235 754.40. It is unknown how many patients with an alternative HCP (n=31) could have received their input. If all 71 patients attended hospital, the estimated cost would be £418 464.00 (Table 4).
Table 4. Theoretical average calculation of NHS budget impact per patient
| Service | Average cost per-patient | Patients (n=31) with alternative community HCP | Patients (n=40) without alternative community HCP | Total patients (n=71) |
|---|---|---|---|---|
| Ambulance | £390.08 | £12 092.48 | £15 603.20 | £27 695.68 |
| Emergency Department care (Category 4) | £717.78 | £22 251.18 | £28 711.20 | £50 962.32 |
| Admission and gastrostomy tube replacement | £4786 | £148 366.00 | £191 440.00 | £339 806.00 |
| Total | £5895.86 | £182 709.63 | £235 754.40 | £418 464.00 |
Discussion
Prior to this service evaluation, published evidence did not exist to support the practice of replacing traumatically displaced feeding tubes in the community setting. This led to varying practices across the UK based on local policies and risk assessments. This service evaluation provides evidence that this practice can be undertaken safely and should help towards standardisation of care for displaced feeding tubes in the community. The results of this service evaluation demonstrate that the implementation of a CHN-led service of gastrostomy tube replacement after traumatic displacement can be undertaken safely, with potential cost savings, when combined with rigorous risk assessment processes and appropriate training.
The primary concern of any healthcare organisation is patient care and safety; as such, any service evolution that involves changes to standard practices requires careful risk assessment, clearly defined processes, training, supervision, documentation and ongoing evaluation. The implementation of the service described here is an example of how a change to standard nursing clinical practice can be approached. Patients were comprehensively assessed by experienced, specially trained CHNs; decisions were guided by clearly defined risk assessment pathways, and every step of the process was overseen by nursing management and carefully documented. In addition, each intervention was closely followed up to ensure it had been successful and resulted in positive patient outcomes.
Historically, the management of HEF patients who experienced a traumatic displacement of their gastrostomy tube has been inconsistent throughout the UK. In some areas, patients would be required to attend acute services for assessment and tube replacement, and in other areas, a community-based, trained HCP would perform the procedure. However, this community practice lacked clinical safety evidence. This service evaluation, conducted over 29 months, reported no clinical complications following 71 tube replacements after traumatic displacement in 60 adult HEF patients with a wide range of diagnoses. This suggests the procedure is low risk for community-based adult patients receiving HEF when performed by a trained CHN with appropriate risk assessment in place.
This service evaluation highlights the value of partnership working between the NHS and third-party healthcare providers to deliver benefits for patients and the wider health service. The pressure on the NHS was heightened by the COVID-19 pandemic but remains at a critical level driven by service provision not keeping pace with population growth, an ageing population, and more people living with long-term medical conditions (Stafford et al, 2018).
In January 2023, the UK government published a delivery plan for recovering urgent and emergency care services, which outlined the need to expand urgent care provided in the community to ensure people can get the care they need at home without requiring hospital attendance (NHS England 2023a), and this shift is also happening in other countries. Emergency departments are not perceived to be the correct setting to manage displaced tubes for patients receiving HEF, who are otherwise medically stable, as it is rarely life-threatening and adds to overcrowding (Barrett et al, 2021). Long waits in emergency departments risk the stoma site healing, resulting in hospital admission and further medical interventions. This service evaluation has demonstrated that, when effectively implemented, the replacement of traumatic displaced feeding tubes is an area of care that can be devolved to community services, preventing hospital attendance, and therefore protecting NHS budgets and resources (Table 4) (NHS England, 2021b). Indeed, analysis of the data from this service evaluation shows an estimated potential cost-saving of £235 754.40 over 29 months based on the 40 patients who would have had no alternative but to access emergency services if their CHN had been unable to replace their tube in the community (NHS England, 2021b).
Although the service evaluation did not measure specific patient or carer reported outcomes, patients benefited from not needing to leave their homes to access acute care, which is a recognised patient preference (NHS England, 2023b). Hospital attendance can be a distressing experience for HEF patients, many of whom have multiple co-morbidities or are immunocompromised. Travel to the hospital for patients with complex needs, potentially long waits in emergency departments, and heightened risk of exposure to infection in the acute setting can generate significant anxiety. In addition, during the period in which this service evaluation was conducted, COVID-19 was a considerable concern, creating further anxiety related to hospital attendance (Fisher et al, 2021).
Limitations
There are several limitations to this service evaluation. First, there were some gaps in the service evaluation data. Not all CHNs documented the reason why tubes were displaced and did not capture the alternative next step for each patient had the CHN not been able to replace the tube in the community. For instance, in some cases, it was not known if there was an alternative community HCP trained to replace feeding tubes, whether they were available and could have visited the patient to perform the tube change, or whether, ultimately, the patient would have required an emergency hospital visit. Similarly, data capture for key variables was inconsistent, such as the volume of water remaining in the balloon of a displaced tube. Such data highlights situations that lead to traumatic displacement, offering the possibility of preventing future tube displacements with additional training and support. Following this service evaluation, revisions have been made to the standard data collection procedure, and this information is now a mandatory requirement. Second, nine patients did not receive a follow-up call within 24 hours due to the procedure taking place on a Friday and the CHN not working over the weekend. This has been addressed, and revisions to the process now ensure that a CHN proactively contacts these patients within 24 hours via an out-of-hours service, including over a weekend or public holiday. Third, it is challenging to accurately estimate the cost of referral to acute care, as patient circumstances and local management can widely vary. Indeed, likelihood of admission will be influenced by factors such as whether the attendance was out of hours (Barrett et al, 2021; however, this is a representative estimate based on the HEF population and excludes other potential costs such as complex discharge management and social care. Finally, as the HEF patient group is extremely diverse from a medical diagnosis perspective, it is difficult to generalise these findings to the entire HEF population and requires ongoing service evaluation and reporting; however, the present findings provide reassurance that community replacement of traumatically displaced gastrostomy tubes is low risk.
Conclusion
The results of this service evaluation of the implementation of a service enabling trained CHNs to replace traumatically displaced feeding tubes in adult patients in the community demonstrate that the practice is low risk, with no clinical complications recorded throughout the follow-up period. These positive results were likely driven by careful risk assessment, clearly defined processes, supervision and appropriate training. This service evaluation also highlights the important role that third-party healthcare providers can play in supporting the NHS to manage patient flow and helping to prevent unnecessary emergency hospital attendances and admissions. Given the primacy of patient safety, the practice of replacing traumatically displaced feeding tubes in the community should continue to be evaluated nationally in the long term. Further research is warranted to explore the patient and carer perspective, including any impact on quality of life, and to explore opportunities to extend this practice to paediatric patients.
Key points
- Home enteral tube feeding is a largely safe practice but is associated with complications that sometimes require acute treatment and interventions.
- Evidence to support the safe practice of replacing traumatically displaced gastrostomy tubes in the community is lacking. This has led to an inconsistent approach to community care for patients across the UK.
- This service evaluation demonstrated that a community homecare nurse-led service to replace traumatically displaced gastrostomy tubes is safe when introduced with highly skilled professionals, vigorous risk assessments and timely follow-up interventions.
- Partnerships between the NHS and third-party healthcare providers can play an important role in improving community care interventions and preventing emergency hospital attendance.
CPD reflective questions
- Can you think of a service innovation in your clinical environment that would improve patient care and experience? What is this, and why is it important?
- What challenges do you think you might face, and how will you overcome these?
- What impact will this service innovation have on patient care and experience?
- How will you monitor the impact of your service innovation on patient care and experience?
- How will this help develop your skills, knowledge and experience as a registered nurse?


