Nursing is a profession historically described as ‘the supreme example of a traditionally women's field’ (Butter, 1989). The Royal College of Nursing (RCN) reported that, as of 2018, 10.7% of nurses were male, although this figure is increasing. The literature is in accord that men are an untapped resource in nursing (McLaughlin et al, 2010; Carte and Williams, 2017), and hiring more males is a viable solution to the global nursing shortage (McLaughlin et al, 2010). The shortage is especially prevalent in the community, where the number of nurses in 2018 had fallen to almost half its 2010 figure (RCN, 2018). Males are even less represented in this area, at less than 5% (Queen's Nursing Institute (QNI), 2019). The discrimination that male community nurses report they feel because of their gender is the highest, at 41%, compared with any other area of nursing (Launder, 2019). Consistent themes appear in the discussion of how to increase male presence in nursing, although some are more pertinent to community nursing. The QNI (2021) appears dedicated to improving inclusion in community nursing by increasing the number of Black, Asian and minority ethnic (BAME) staff. This drive should also extend to increasing male presence in community nursing.
The profession of district nursing originates in 1859, with William Rathbone, a Liverpool merchant who employed a nurse to care for his wife at home as she approached the end of her life (QNI, 2020a). Florence Nightingale went on to work with Rathbone to develop nursing schools catering to delivering care across districts in Liverpool, and soon, nationwide. It was Nightingale's work that allowed the QNI to legitimise the profession of district nursing in 1887 (Kelsey, 2016). The role began with four key principles, ones that still exemplify the importance of community nursing today: patients often prefer to be treated in their own environment, long-term conditions are better managed at home, hospital resources are finite and home care is cheaper than hospital care (Cook, 2010). Undoubtedly, the profession owes Nightingale a lot.
Data are clear that nursing remains a largely female-dominated job. However, this was not always the case. Female dominance in nursing only began in the nineteenth century (Bullogh, 1994). During this time, Nightingale's reforms altered the culture of nursing. She reported that male hands were ‘rough’ and ‘not fitted to touch, bathe and dress wounded limbs’ (Brown et al, 2000). She believed it would not be appropriate for a man to be a nurse, a notion that is not entirely absent today (DeVito, 2016). There was a clear stigma against men working in a caring environment at this time (Bullogh, 1994). However, prior to this, the role of the male nurse was far more significant, principally due to the relationship between nursing and the military (Ross, 2017). Nursing education is reputed to have been born in India in 250 BC, and only men were granted access because of their ‘pureness’ (Vallano, 2011). During the fourth century when the Byzantine Empire, fuelled by the ascendancy of Christianity, was growing from its pagan Roman roots, the first institutionalised hospitals were created by Constantine the Great. It was in these hospitals that nurses emerged as a distinct and separate entity to physicians-wards were gender specific with the male wards being staffed solely by male nurses, and female nurses looking after the female wards (Bullogh, 1994). Nevertheless, Bullogh (1994) did concede that this was far from the norm, and, in other cities away from the East, nurses were far more likely to be solely male. It is evident that the care of the unwell was deemed to be something only men were fit for, and women were simply not suited to the task (Bullogh, 1994). This gender inequality seems to go on to define the history of nursing, even from its nascence.
Through the Middle Ages, religion had a strong hold over nursing, as caring work made up a large part of what those in a religious order were expected to do. Thus, approaching the middle of the nineteenth century, nursing was perceived as something only those in religion took part in (Bullogh, 1993). It was Nightingale who eventually broke this centuries-held perception, but, in doing, so she conflated the role of nursing and the caring, nurturing personality still seen today. However, not unwittingly, she also pushed the idea that these traits could only be possessed by a woman due to their fundamental nature as mother and nurturer (Bullogh, 1994). This change in the way of thinking about nursing led to its status as a female-dominated job today (Brown et al, 2000).
From the Crusades of the eleventh century to the Franco-Prussian War, history tells of a long and constant relationship between men and the profession of nursing (Bullogh, 1994; Ross, 2017). It was, in fact, men that made up the vanguard of caring work throughout history up until the nineteenth century when, prompted largely by Nightingale, nursing began to become a primarily female occupation (Brown et al, 2000). Nevertheless, during both World Wars, male nurses played an active role in service. Most notably, in World War II, as women were not allowed on the frontline, male nurses served with immense bravery, skill and dedication (Ross, 2017). Yet, it seems this part of history regarding the male nurse has been forgotten. In spite of men's long history with nursing, their place in has been largely ignored by society-a key reason for this being the female movement of the nineteenth century that has skewed the profession's history (Mackintosh, 1997). In accounts of male nurses after that movement, in the early twentieth century, the male was seen as inferior by their female counterparts, treated with hostility and faced obstacles to employment, as well as having negative stereotypes about them spread (Mackintosh, 1997; Ross, 2017).
Evans (2004) suggested that it is this ignorance of the male relationship with nursing that has caused the male nurse now to be perceived as an anomaly. This had resulted in the male nurse lacking any knowledge about the importance of their professional and historical background. Given that men do represent a large and significant role in the history of nursing, perhaps more education should be delivered today around the profession's roots and development, and the male position in this. This recollection of history might encourage more men to enter into nursing and dispel some of the stigma for those already in it.
Accounts are rare of the male and female nurse working in tandem. Nightingale's feminist reforms in the nineteenth century signalled such a dramatic shift in nursing that male nurses were stigmatised and considered to lack the emotion or compassionate nature to care for the sick. In the decades after this, male nurses were paid less and treated with hostility by their female peers, even being referred to as orderlies despite possessing the same diploma and level of training (Office of Medical History, 2016). Although much of this is to do with the fundamental gender discourse that permeates society throughout history, it would be imprudent to not acknowledge the fact that nursing has never been perceived as gender neutral (Ross, 2017).
There is an argument to suggest that Nightingale had other effects on today's face of nursing as well, namely, the subservient role that nursing plays in medicine, and this relationship only highlights the societal trend of males possessing more power than females (MacMillan, 2012). Jinks and Bradley (2004) argued that the depiction of Nightingale as the paragon of tenderness reinforced the stereotypical image of a nurse as nothing more than a handmaiden. When Nightingale developed her nursing school, in order to gain support from physicians for the idea, she instructed nurses to answer to physicians and obey them in all medical matters (MacMillan, 2012). Furthermore, while Nightingale accepted that some women would pursue medicine in favour of nursing, she considered that they should focus their care on women's and child's health (MacMillan, 2012).
Negative stereotypes have been blamed as the primary reason for male underrepresentation in nursing today (Stanley et al, 2016). Nightingale's acceptance that nursing would be a subservient profession to medicine has ramifications, as, historically, the division of influence between nursing and the male-dominated medicine was based on gender alone (Jinks and Bradley, 2004). This power imbalance still exists and could lead to feelings of reduced masculinity for any male entering nursing. Furthermore, male community nurses are often mistaken for doctors (Stanley, 2012). Society grants more power to men, and when seeing a male medical professional, it is easy to mistake them for a doctor, which is the more powerful of the two professions (Fenkl, 2006). However, this mistake compromises the nurse's ability to function in their role (O'Lynn and Tranbarger, 2007).
Even after Nightingale's reforms, healthcare was very hierarchical, with one source comparing it to a Victorian family-the physician as the dominant father and the nurses as compliant children (Helmstadter and Godden, 2014). Even today, nursing struggles to gain recognition as a partner profession to medicine rather than an obedient one (Sorensen et al, 2008). It is Nightingale's decision to instruct nurses to be submissive to physicians that has to be seen as a flaw in her nursing revolution. Yet, it is impossible to say where nursing would be now if that decision had not been made, and, as MacMillan (2012) indicated, the decision was driven by a sense of pragmatism rather than any disinclination to follow through with her ambition of gaining increased power for women. The decision was made to acquire the support of the physicians for her nursing school, and, if such an action had not been taken, then the nursing school might never have come to be, or nursing might have ended up differently today. Nelson and Rafferty (2010) called for more credence to be given to Nightingale's vision and for modern readers to interpret her pivotal decision differently. They argued that, in promising nurses' obedience, she may not have meant the complete servility that is understood today. Despite that, it is difficult to argue that her decision has not influenced the relationship between nurse and doctor, and the historical roles of woman and man, even today.
Nightingale purported the view that men were unsuited for caring roles because they are not tender by nature, and this view appears to have been consolidated today. Nursing is an intrinsically caring profession, yet this caring nature is incongruent with Western society that encourages men to keep expressions of emotions hidden (Ierardi et al, 2010). Nightingale alleged that females are more suited to nursing due to their compassion, and decades of stereotypes around the stoic, tough male have consolidated the view that men should not be in caring roles such as community nursing (Larocco, 2008).
Men tend to lean towards more ‘technical’ areas of nursing, such as critical care and surgery (Carte and Williams, 2017) and are less common in areas where a high level of compassion and emotional intelligence are perceived to have a higher importance (Juliff et al, 2016). The prevalence of palliative care and the importance of the fostering of a therapeutic relationship in the community would perhaps substantiate this notion. It is suggested that men want to avoid uncomfortable or embarrassing situations around intimate touch and, as such, gravitate towards ‘low-touch’ areas (Harding et al, 2008; MacWilliams et al, 2013), but intimate touch is a common feature of community nursing, for example, during procedures such as wound care and catheterisation (QNI, 2015). Male nurses worry that their caring behaviour is often misconstrued as sexual impropriety (Ierardi et al, 2010). This sexualisation of the male nurse can lead to feelings of suspicion and rejection, compromising their ability to deliver care (Evans, 2002). Societal attitudes towards female touch are focused on tenderness and compassion-essential to nursing care-yet male touch is frequently sexualised (Harding et al, 2008). Community nursing is a role that demands a degree of tactility, and so this further complicates the role of the male, more so than in other areas of nursing. It can also lead to a cautionary approach when touching a female patient, allowing their care to appear superficial and the nurse themselves as insincere (Inoue et al, 2006). It is suggested that feelings around human touch are relative to the wellness of a patient: the more unwell a patient is, the more human touch is considered comforting and nurturing; yet, as the patient recovers, those same actions can be misunderstood as sexual (Chiarella and Adrien, 2014). Acknowledging this, the confusion about the touch of male community nurses becomes conflated when it is considered that the patients they see will generally not be as acutely unwell as those in hospital.
The trend of men feeling that their careers are steered in certain directions, away from areas such as paediatrics and gynaecology, is not a new one (Stanley et al, 2016). The excitement of ‘never knowing what is coming through the door’ was offered as the reason for one group of male nurses' preference for more technical areas, such as critical care (Juliff et al, 2016). More publicity should be granted to the variety and complexity of a community nurse's role, as well as its fast-paced nature and the autonomy with which a community nurse works, to increase its attractiveness to men. Despite male tendency to gravitate towards certain areas of nursing, the literatures agrees that men have a distinct advantage when it comes to career prospects (McMurry, 2011). Just over one-in-10 UK nurses is male, yet males occupy one-in-four band 8 and above job roles (NHS, 2018) (Figure 1).
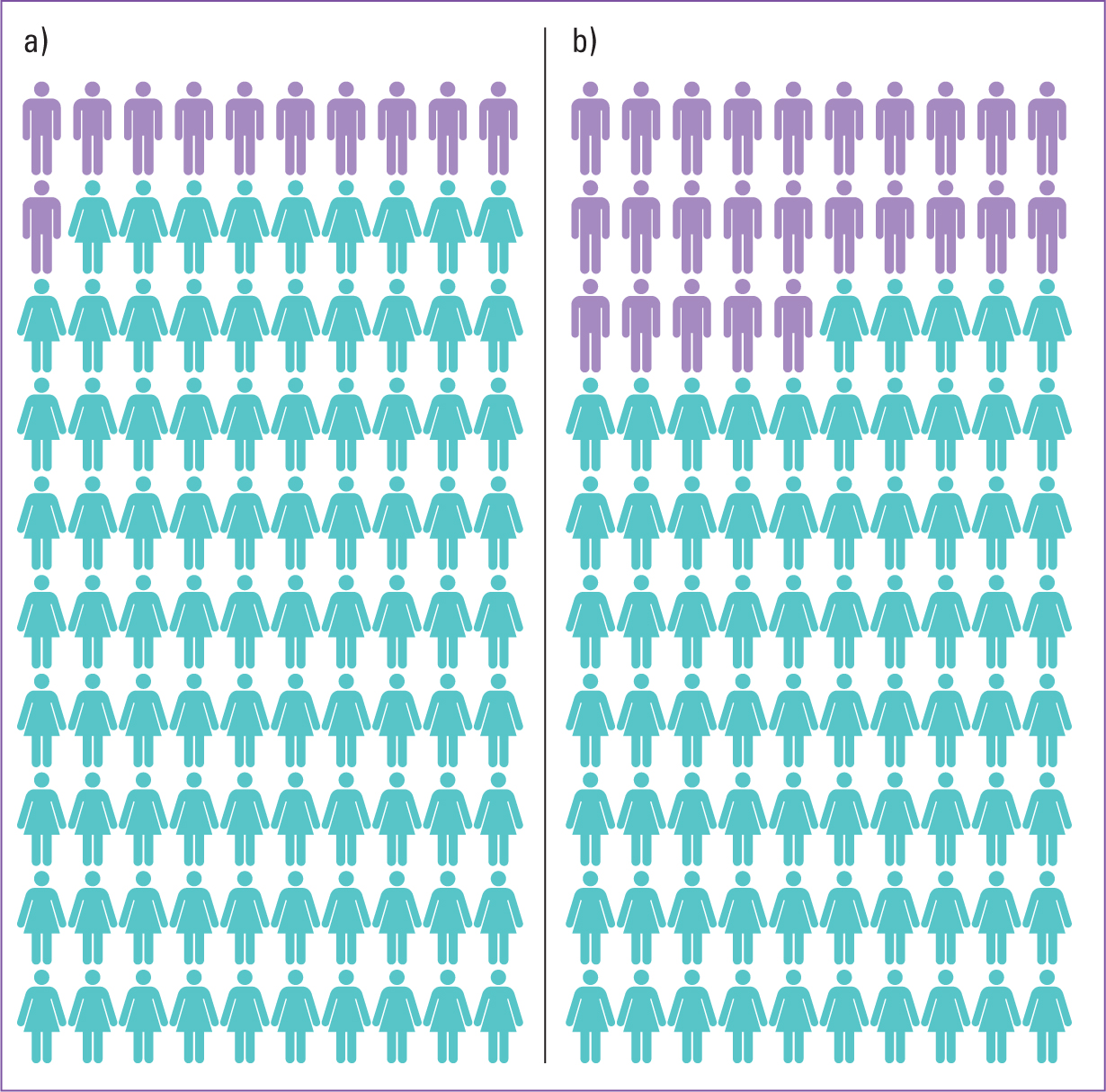 Figure 1. (a) Gender ratio of UK nurses. (b) Ratio of UK nurses at Band 8 or higher
Figure 1. (a) Gender ratio of UK nurses. (b) Ratio of UK nurses at Band 8 or higher
This disparity has been blamed on the ‘glass escalator effect’ (McMurry 2011), invisible pressures because of which men feel they are being forced to progress. Kleinman (2004) suggested that men are valued in nursing simply due to their shortage. This tokenism would seem to neglect any qualities the male candidate possesses in favour of their gender. There is evidence to suggest that men progress more quickly in nursing because they possess more ambition for professional power (Boughn, 2001; Kleinman, 2004). However, this disregards the female nurses who possess the same ambition.
Historically, women were forced to choose between career advancement and family, with the former perceived as unfeminine (Fels, 2004). Yet, in a society where women are attaining positions of power more than ever before (Paxton and Hughes, 2017), the prevalence of male nurses at higher level positions compared with the number in entry-level positions is stark. Van Vianen and Fischer (2010) reported work-home conflict as barrier to female progression in nursing, and concerns over childcare, maternity leave and career breaks have all been considered to explain male nurses' advantage when it comes to progressing (Baumgartner and Schneider, 2010). Evidence highlights difference motivating factors in career choices between the genders-women prefer job fulfilment and men prefer opportunities to progress and financial stability (Stanley et al, 2016). Considering this, nursing's societal reputation as an underpaid job (Goodare, 2017) should be deemed a reason for male underrepresentation in nursing.
Media portrayals have a huge influence on societal opinion towards nurses (Stanley et al, 2016). The community nurse is typically portrayed as a maidenly character on a bicycle. Other media portrayals feature a battle-axe character or sex object (Jinks and Bradley 2004). Crucially, most nurses in the media are female, and the vast majority of male nurse portrayals were disparaging – incompetent, murderous, corrupt or effeminate (Stanley, 2012). Research illuminates this is a real problem for men when choosing their career path, they fear by entering nursing they are abandoning their masculinity (Juliff et al, 2016).
It is reported that female nurses feel safer working alongside a male where there is a threat of sexual harassment or violence (Riddell, 2011). The community nurse's status as a lone worker means that adding a male to the team could positively affect the dynamics. However, any employers considering this notion should be aware of pigeon-holing men into the ‘muscle’ role, as 58% of male nurses report experiencing this perception (Stanley et al, 2016). This could lead to men feeling forced into situations they feel ill prepared for based purely on their gender, such as fixing equipment or monitoring potentially violent patients, engendering feelings of prejudice (Meadus and Twomey, 2011).
Conclusion
NHS England (2014) highlighted the need to break down the traditional divide between healthcare in hospitals and the community, and the increasing need for community nurses means they are at the forefront of this movement (QNI, 2020b). Therefore, community nursing has an obligation to use the untapped resource of male employment to increase staffing numbers. The QNI (2021) is motivated to improve the equality and inclusion in the community nurse workforce, and as well as increasing the amount of BAME staff, this also means more should be done to create opportunities for men. Furthermore, nursing leaders have vowed to make the nursing workforce more representative of the society they serve (Carte and Williams, 2017). However, tangible strategies to increase male presence in nursing appear scarce. Media portrayals and perceptions of compromised masculinity have been blamed on the low number of male nurses, and males' preference for ‘low-touch’ areas is one reason for their underrepresentation in community nursing. More should be done to combat the stigma around male touch, and more credence should be given to the caring nature of men. Similarly, more needs to be done to highlight the changing nature of the community nurse role and the increasingly fast-paced and technical duties entailed. Female nurses themselves receive negative gender bias, as in most aspects of society, and more should be done to combat gender inequality in the workplace (Bruckmüller and Braun, 2020). Further research is required into how better to increase the numbers of men in nursing, particularly community nursing, where the shifting dynamics of the role has led it to become an increasingly technical job.
KEY POINTS
- The modern nursing workforce is greatly skewed towards the female gender
- A reason for this could be the historic view that women are more suited than men to the role of caring and nurturing, and men have usually been considered better suited to more technical roles
- One way to overcome staffing shortages in community nursing and other fields of nursing would be to encourage the inclusion of men
- Gender stereotypes around masculinity, and community nursing's emergence as an increasingly technical role need to be considered
CPD REFLECTIVE QUESTIONS
- With the balance between hospital care and community care shifting towards the community, what can be done to increase the community nursing workforce?
- Why are men so underrepresented in community nursing more so than in other areas of nursing?
- How much of a role does the media play in purporting gender stereotypes around men, and nurses in general?


