Over 4 million people in the UK are known to have diabetes mellitus. The most common form of diabetes is type 2, which is preventable and treatable (Diabetes UK, 2023a). Most people with type 2 diabetes are managed in primary care until complications develop (McCombie et. al, 2017). COVID-19 restricted access to routine diabetes care, limiting new diagnoses, affecting self-management, routine follow-ups, access to medications and affected lifestyle (Khunti et al, 2022). The lack of support has affected the ability of people with diabetes to manage their condition well (Diabetes UK, 2023b).
This article will explore the diagnosis and treatment of type 2 diabetes using a case history approach.
Diabetes is defined as:
‘…a chronic, metabolic disease characterised by elevated levels of blood glucose (or blood sugar), which leads over time to serious damage to the heart, blood vessels, eyes, kidneys and nerves.’
(World Health Organization (WHO), 2021a)
In the past 80 years, the number of people in the UK with a diabetes diagnosis has risen from 200 000 to around 4.3 million (Diabetes UK 2023a). Figure 1 illustrates this.

Diagnosis of type 2 diabetes
Ms Martha Samuel is a 39-year-old woman of Afro-Caribbean ethnicity. She complains of being hungry, thirsty and tired. She reports that she has to wake up twice at night to pass urine. These are classical, clinical features of diabetes (Table 1).
Table 1. Clinical features of diabetes (Nazarko, 2016)
| Symptom | Reason |
|---|---|
| Polydipsia – excessive thirst | The body tries to reduce sugar levels by passing more urine. The person drinks more to replace lost fluid. |
| Polyuria – increased urine output | The body tries to reduce sugar levels by passing more urine. |
| Polyphagia – increased appetite accompanied by weight loss | The body is unable to use glucose effectively and the person feels hungry. |
| Tiredness and irritability | The process that converts glucose into Adenosine triphosphate (ATP) and provides energy to the cells is affected. High blood sugar prevents the body drawing on reserves of glycogen in the liver. |
| Fungal infection | High sugar levels in blood and tissues increase infection risks. |
| Poor wound healing | High sugar levels affect the circulation and slow wound healing. |
| Deterioration of vision | High sugar levels affect vision |
Note: Adapted from Nazarko (2016)
Ms Samuel is 157 cm in height and weighs 99 kg. Her body mass index (BMI) is 40.1, which is stage 3 obesity, also referred to as morbid obesity (NICE, 2014). Table 2 illustrates the interpretation of the BMI index.
Table 2. Body mass index interpretation
| Body mass index | Comments |
|---|---|
| 18.5−24.9 kg/m2 | Normal weight |
| 25−29.9 kg/m2 | Overweight |
| 30−34.9 kg/m2 | Obesity I |
| 35−39.9 kg/m2 | Obesity II – may be referred to as ‘morbidly obese’ |
| >40 kg/m2 | Obesity lll – may be referred to as ‘super obese’ |
Note: Adapted from Weir and Jan (2023)
According to Ms Samuel, she gained weight over the last few years but has lost around 8 kg in the last few months. Her urinalysis test tested strongly for glucose. There were no ketones in the urine.
The National Institute for Health and Care Excellence (NICE) (2023a) guidance recommends testing for diabetes if a person has risk factors and/or has clinical features of diabetes. Risk factors for type 2 diabetes include age, ethnicity, gender, socioeconomic deprivation and obesity. Socio-economic deprivation doubles the risk of diabetes (Stringhini et al, 2016). Ms Samuels is a registered nurse who works as a ward manager and therefore, is not socioeconomically deprived.
Ms Samuel is from the West Indies; her Afro-Caribbean heritage means that her risk of developing type 2 diabetes is twice that of a Caucasian woman. This is thought to be due to Afro-Caribbean people carrying excess weight around the abdomen and having increased insulin resistance (Misra, 2015). Other factors such as a reduced β cell function may contribute to risk (Pitts-Tucker, 2012).
The risk of diabetes increases with age due to individual factors and age-related changes (Hermann et al, 2021). Ms Samuel is young; she is not yet 40 years. People who develop type 2 diabetes under the age of 40 years are more likely to experience rapid deterioration in pancreatic function and have a greater incidence of adverse outcomes (Magliano et al, 2020).
Type 2 diabetes is associated with obesity and Miss Samuel has stage 3 obesity (WHO, 2021b).
A HbA1c blood test is often used to diagnose or monitor diabetes; it measures the amount of glucose attached to the haemoglobin over a 2–3 month period as this is how long the blood cells typically last for in the body (Medline Plus, 2021). The higher the HbA1c, the greater the risk of developing diabetes-related complications. Table 3 illustrates how HbA1c correlates with average blood glucose levels (Seery, 2023).
Table 3. HbA1c and average blood glucose
| HbA1c (mmol/mol) | Average blood glucose (mmol/L) |
|---|---|
| 119 | 18 |
| 108 | 17 |
| 97 | 15 |
| 86 | 13 |
| 75 | 12 |
| 64 | 10 |
| 53 | 8 |
| 42 | 7 |
| 31 | 5 |
NICE states that if the person has symptoms of diabetes and an HbA1c greater than 48 mmol/mol, diabetes can be diagnosed (NICE, 2023a). HbA1c is not suitable for people with conditions affecting haemoglobin such as sickle cell disease, chronic kidney disease and people on haemodialysis. It should not be used during pregnancy. When HbA1c is not suitable, a test measuring glycated albumin may be used (Zendjabil, 2020).
Ms Samuel had an HbA1c of 98, indicating an average blood glucose level of around 15 mmol/l.
How diabetes affects health and wellbeing
Ms Samuel feels very unwell. This is common in people with undiagnosed or poorly managed diabetes. High blood glucose levels cause lack of energy and increased risk of tissue damage.
Type 2 diabetes, once a disease that affected middle aged and older people, is increasingly affecting younger adults and children (Romieu et al, 2017). Patients like Ms Samuel, who present with weight loss at onset of diabetes, high HbA1c and young onset age, are more likely to develop ketosis and require careful monitoring (Dong et al, 2023).
Undiagnosed or poorly managed diabetes is associated with premature death. As a 40-year-old women, Ms Samuel's life expectancy is 10 years less than a woman of her age who does not have type 2 diabetes (Emerging Risk Factors Collaboration, 2023).
Diabetes can also lead to problems with vision and circulation, and increases the risk of heart disease, stroke, dementia, nerve damage and sexual difficulties (NICE, 2022).
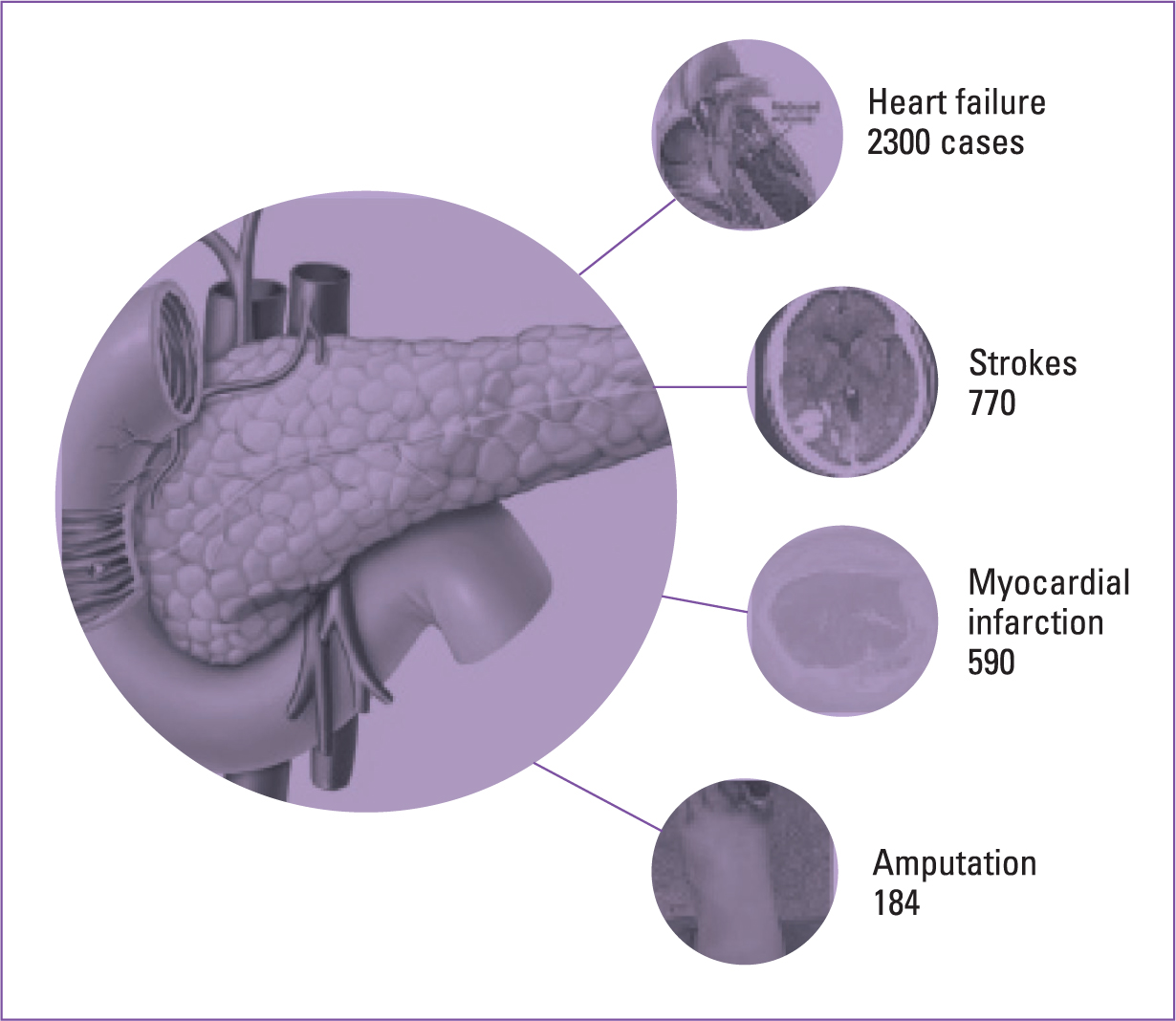
The main complications of diabetes are microvascular disease affecting the eyes, nerves and kidneys, and macrovascular disease leading to cardiovascular disease, cerebrovascular disease and lower-extremity artery disease (Chawla et al, 2016).
Every week, diabetes leads to 184 amputations, more than 770 strokes, 590 heart attacks and 2300 cases of heart failure (Diabetes UK, 2023a) This is illustrated in Figure 2.
Treatment options
Miss Samuel has two risk factors; one of them—obesity—is modifiable, and the other—ethnicity—is not. The priority was to treat her diabetes symptoms by reducing her blood glucose. Figure 3 based on NICE guidelines (2014) outlines treatment options.
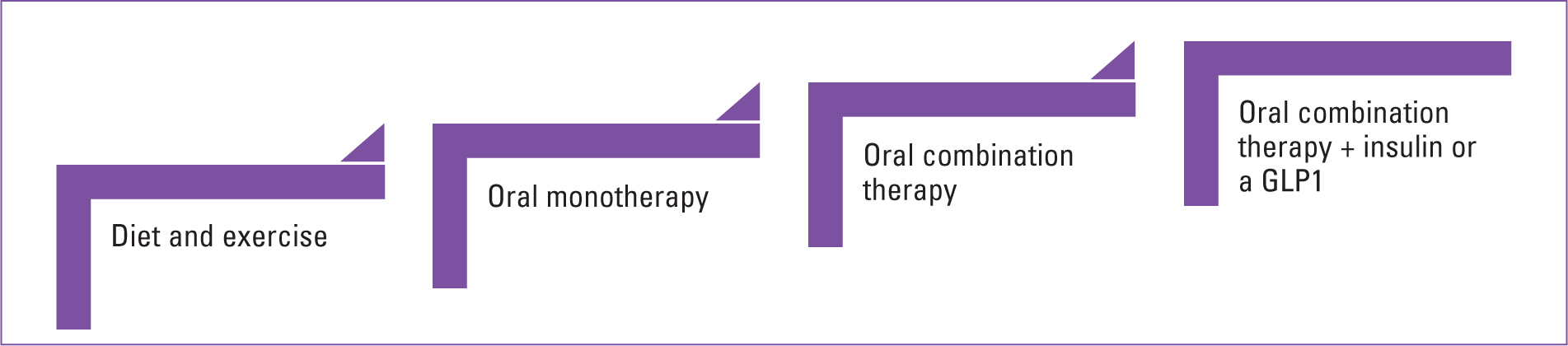
The guidelines show a stepwise approach to diabetes management and in an ideal situation, we would start at the bottom and work our way up in terms of treatment. This is not going to be possible with Ms Samuel as she is symptomatic and her obesity indicates a high level of insulin resistance. Ms Samuel will require a combination of diet, exercise and two medications to treat her diabetes.
Diet
We are in the midst of a revolution in the way we treat type 2 diabetes. Research demonstrates that weight loss can enable many people with type 2 diabetes to go into remission. The Diabetes Remission Clinical Trial showed that 86% of people who had been diagnosed in the previous 6 years with type 2 diabetes could achieve remission if they lost weight rapidly. In overweight and obese people, the greater the weight loss, the higher the level of remission. A loss of 15 kg led to 86% remission and a weight loss of 10 kg led to a 46% remission (Lean et al, 2018).
This study led to the NHS England introducing a programme to enable people with type 2 diabetes to lose weight and put their diabetes into remission. The NHS Type 2 Diabetes Path to Remission Programme (formerly known as the NHS Low Calorie Diet Programme) is being rolled out across England. It provides a meal replacement programme called ‘soups and shakes’ for 3 months. These provide around 900 calories daily. The programme also provides ongoing support from clinicians and coaches to help people maintain healthy lifestyles (NHS England, 2022). Scotland and Wales have similar programmes (Counterweight, 2022; NHS Lanarkshire, 2023). Pregnant women are not eligible for the weight loss programmes. Table 4 provides details of eligibility.
Table 4. Criteria for referral for NHS type 2 diabetes Path to Remission Programme
| Criteria | Details |
|---|---|
| Age | 18−65 |
| When diagnosed | Within the last 6 years |
| BMI |
|
Ms Samuel was very keen to try the soups and shakes diet. She commented that it seemed to be exactly the same as the ‘Lighterlife’ total fast plan. Ms Samuel has a friend who used this plan.
She reported that her friend had spent almost £900 on the 12-week plan and had lost a stone in weight each month. Ms Samuel was delighted to be offered this plan for free.
Medication
There are a number of different classes of medication that can be used to treat type 2 diabetes; these are, biguanides, sodium glucose cotransporter 2 (SGLT2) inhibitors, DPP-4 inhibitors, glitazones, sulphonylureas and insulin. Ms Samuel has an HbA1c of 98 indicating a blood glucose of around 15 mmol/mol. She is symptomatic. At this point, the aims of treatment are to reduce blood glucose levels and relieve symptoms. The treatment options are a biguanide, metformin and a sulphonylureas or insulin as a secondary medication.
Biguanides
Metformin, is a biguanide class drug. It was developed from Galega officinalis (goat's rue or French lilac) and was used in herbal medicines for centuries. It is normally used as a first-line of treatment in type 2 diabetes. It reduces the amount of glucose released by the liver and allows cells to take in glucose by reducing insulin resistance. It also helps to reduce the risk of heart disease
Metformin does not cause hypoglycaemia when used as monotherapy. It can lead to weight loss (3–5% of body weight), and it has been shown to decrease plasma triglycerides concentration (10–20%) (Nazarko, 2023).
The most common side-effects of metformin are diarrhoea, nausea and abdominal discomfort. The starting dose is 500 mg daily. It is titrated gradually to reduce the risk of gastrointestinal side-effects, starting at 500 mg with breakfast and increasing by 500 mg in weekly intervals until a dose of 1000 mg with breakfast and dinner, or 2 grams MR once daily with breakfast, is reached (NICE, 2023b).
Metformin begins to lower blood glucose within a few days but it can take around 3 months for it to be fully effective (Drugs.com, 2023). Metformin can cause life-threatening lactic acidosis. This is rate (<1 in 100 000). Lactic acidosis is caused by a build up of lactic acid. Side effects of metformin include lactate production, reduced lactate clearance, and the risk of metabolic acidosis. Metabolic acidosis generally occurs in overdosage or in the presnence of acute or chronic illness. Conditions that increase lactic acidosis include acute or chronic renal disease, hepatic or heart failure, shock and critical illness (Dyatlova et. al, 2023). Metformin should be used with caution in people with renal failure. The dose should be reviewed when estimated glomerular filtration rate (eGFR) falls below 45 mL/min and should not be used when eGFR is 30 mL/min or below (NICE, 2023b).
Ms Samuel agreed to take metformin. We explained that she would require an additional medicine to reduce her blood glucose as metformin takes a long time to work and is sometimes insufficient to control blood glucose. The options for a second agent were insulin or a sulphonylurea. Ms Samuel was shocked at the suggestion of insulin. She said, ‘That sounds very serious. I thought I had mild diabetes, are you sure its necessary?’
Type 2 diabetes, in common with type 1 diabetes, can have devastating effects on a person's health and well being. It is important that the public and health professionals are aware of this (Diabetes UK, 2023c).
Ms Samuel really did not want to have a daily injection of long-acting insulin so we needed to consider a sulphonylurea.
Sulfonylureas
There are five sulfonylureas: glibenclamide, gliclazide glimepiride: glipizide and tolbutamide (NICE, 2023c). Sulfonylureas stimulate the β-cells in the pancreas to produce more insulin and decrease clearance of insulin by the liver. They are only effective if there are functioning pancreatic β-cells sulfonylureas can cause hypoglycaemia. Sulphonylureas lead to weight gain, so long-term use is best avoided in people who are obese.
Ms Samuel's was prescribed gliclazide 40 mg each morning. This can be increased to 80–160 mg daily; doses higher than 160 mg to be given in divided doses; maximum 320 mg per day.
The aim was to use the gliclazide to stabilise blood glucose and treat symptoms. When this occurred, then the medium term plan was to commence a SGLT2 inhibitor and stop the gliclazide. This would eliminate the risk of hypoglycaemia and help reduce weight.
Sodium glucose cotransporter 2 inhibitors
Ms Samuel is obese and the medium term aims in relation to her diabetes were to manage blood glucose, minimise symptoms of diabetes and facilitate weight loss. Ms Samuel is at high risk of cardiovascular disease.
NICE (2022) guidelines recommend that if the person with diabetes who has been prescribed metformin also has heart failure, cardiovascular disease or risks of either, an SGLT2 should be prescribed in addition to metformin. Metformin should be initiated first and the SGLT2 then added when the person is stabilised on the first medication.
There are four SGLT2s available: dapagliflozin, canagliflozin, empagliflozin, ertugliflozin (NICE, 2023d). SGLT-2 enables the proximal renal tubules in the kidneys to reabsorb around 90% of glucose from tubular fluid. SGLT2 inhibitors block the reabsorption of glucose by the kidney, and increase the amount of urine excreted by the kidney. This reduces blood glucose levels in people with diabetes who have elevated blood glucose levels. SGLT2 inhibitors work independently of insulin and can be used in combination with insulin. They reduce major adverse cardiovascular and cerebrovascular events, such as stroke, myocardial infarction and cardiovascular death, as well as the number of hospital admissions for heart failure (Zelniker et al, 2020).
Common side-effects include candida infection, back pain, increased amount of urine passed, dizziness and a mild skin rash. Serious, life-threatening, and fatal cases of diabetic ketoacidosis are rare in people with type 2 diabetes. Gangrene (necrotising fasciitis of the genitalia or perineum) is a rare, but serious, and potentially life-threatening infection, and has been associated with the use of SGLT2 inhibitors.
Patient progress
To date, Ms Samuel has lost around 15 kg; however, she is not sure if she can keep things up. She is now taking metformin MR 2 grams and dapagliflozin 10 mg each morning. She is 32 kg above her target weight and is requiring a lot of support to maintain a healthy diet. She reports that she feels so much better. She is asking if she can have a glucagon-like peptide 1 (GLP-1) receptor agonists such as semaglutide to help curb her appetite. The use of GLP-1 receptor agonists will be discussed in a future article.
Conclusion
Healthcare staff are not always good at looking after themselves. A study found that 25.1% of registered nurses and 31.9% of unregistered healthcare workers were obese (Kyle et al, 2017). A recent study shows a high global prevalence of obesity and overweight among nursing staff. The authors state that healthcare organisations and policymakers should improve working conditions and environments for nurses to better maintain their metabolic health (Sadali et al, 2023).
NHS England (2023b) has a digital weight management programme and 15 000 staff have been supported over 3 years. We need to do much better.
NHS and primary care employers need to become much more proactive and help nursing staff to maintain and regain metabolic health.
Key points
- People with diabetes have struggled to manage diabetes in the last few years
- Diabetes diagnoses have been delayed and support has been suboptimal
- Community nurses can help support people with diabetes to manage the condition as well as possible
- As nurses, we must remember to look after ourselves as well as our patients
CPD reflective questions
- What factors have led to the increase of diabetes over the last 30 years?
- Why do you think people with diabetes have struggled to manage their condition in the last few years?
- How can you support people with diabetes to manage their condition well?


