The term ‘stoma’ is used to describe an opening on the surface of the abdomen which has been surgically created to divert the flow of faeces or urine. People who have had stoma surgery are sometimes known as ‘ostomates’ (Colostomy UK, 2024).
There are around 177 000 people in the UK with a stoma (Kettle, 2019). It is estimated that one in 335 adults has a stoma (NHS Inform, 2024a). Stomas are created because of a number of conditions that affect the small and large intestine. In the UK around 6400 permanent colostomies are created each year (NHS Inform, 2024a). Ileostomies are more common and around 9000 are created annually in England (NHS Inform, 2024b).
The person who has a stoma may require help and support from the community nurse upon discharge from hospital for months, or even years to come. The community nurses needs to have a good understanding of the anatomy and physiology, its indications and common complications.
Anatomy and physiology
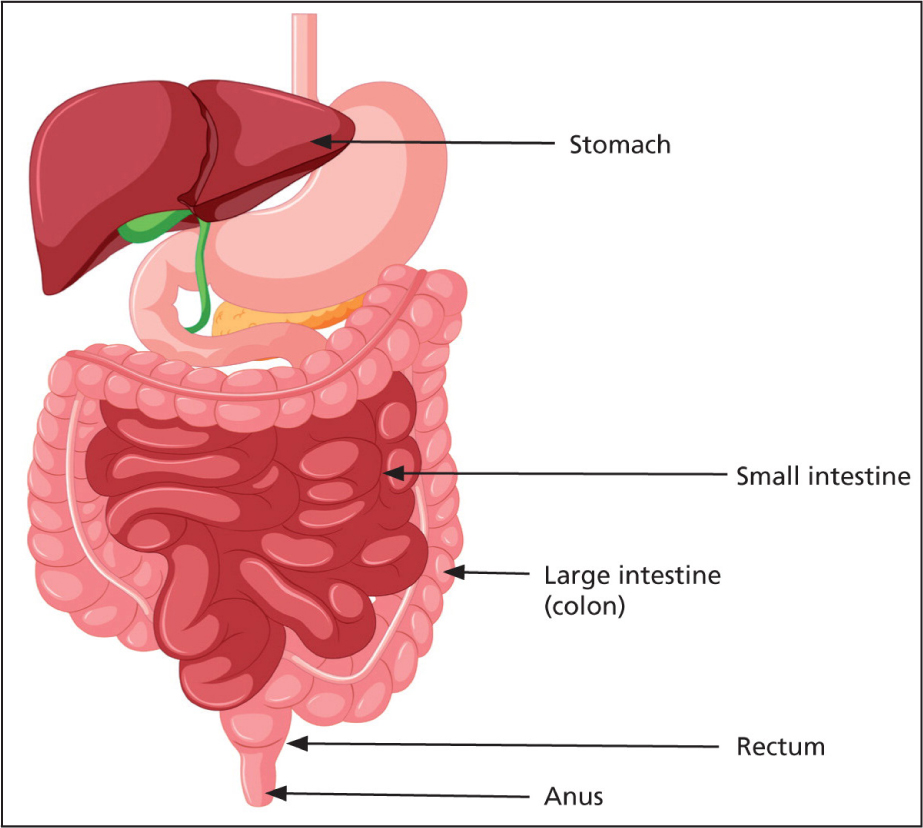
The small intestine extends from the pyloric sphincter of the stomach to the ileocecal valve (Figure 1). It is 4–6 metres long and consists of three segments: the duodenum, the jejunum and the ileum.
The small intestine breaks food down so that nutrients can be absorbed, and reabsorbs water and moves food residue into the colon. It is an alkaline environment and has low levels of healthy bacteria. This protects the body from harmful bacteria (Kastl et al, 2020).
Blood supply to the duodenum is from the superior and inferior pancreaticoduodenal arteries. The superior mesenteric artery supplies the jejunum and ileum (Greenwood-Van Meerveld et al, 2017; Tortora and Derrickson, 2017; Collins et al, 2023).
The large intestine extends from the ileocecal valve to the anus (Figure 1). It is around 1.5 metres long and consists of the ascending, transverse, descending and sigmoid colon, rectum, and anal canal (Tortora and Derrickson, 2017). The colon has four basic functions. These are reabsorption, creation of vitamins and biotin, formation, storage and elimination of faeces. The colon reabsorbs up to around five litres of water in 24 hours. It also reabsorbs bile salts that have been secreted from the liver to enable digestion to take place. Bacteria in the colon form three substances: vitamin K, necessary for blood clotting; vitamin B5, required for the manufacture of neurotransmitters and hormones; and biotin, a substance that is important in glucose metabolism. The colon eliminates toxins from the body. It eliminates the indigestible residue of food and excess metabolites. As the end products of digestion pass through the colon, they become thicker and more formed. The colon's end product faeces contain around 100 ml of water and is stored in the colon until it can be eliminated (Nigam et al, 2019).
The superior mesenteric artery supplies blood to the caecum to the distal transverse colon. The inferior mesenteric artery supplies the distal transverse colon to the rectum.
Ileostomy
An ileostomy is formed by bringing a part of the ileum onto the surface of the abdomen (Figure 2). Ileostomy may be carried out as an emergency or an elective procedure. Indications for this are intestinal obstruction due to benign and malignant disease, perforation peritonitis, ulcerative colitis, Crohn's disease and mesenteric ischemia (Pandiaraja et al, 2021).
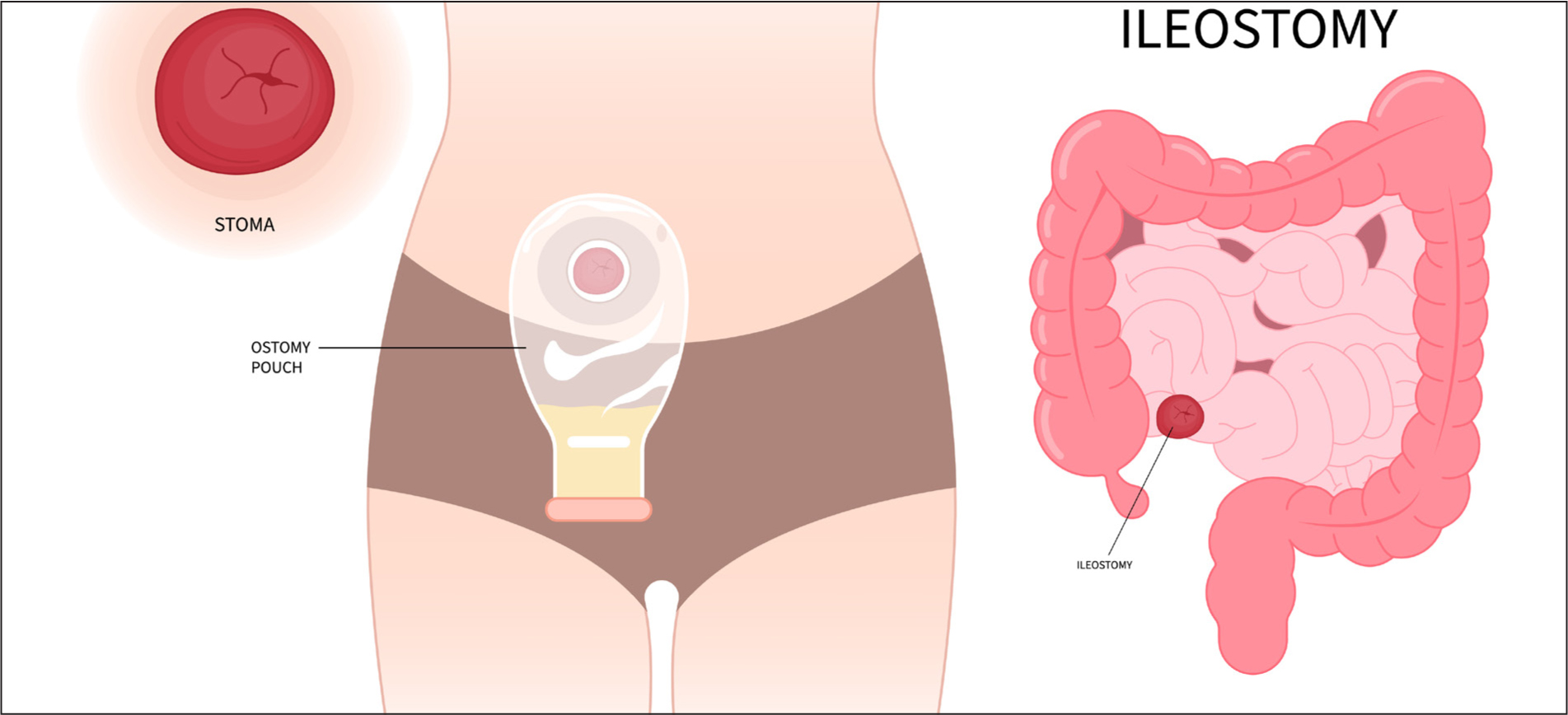
The ileostomy is normally located in the right iliac fossa. Stomal output is related to the site of the stoma and is affected by diet and fluid intake, medication and health conditions. Consistency of output ranges from very soft and porridge-like, to fluid. Ileostomy output ranges from 500–800 ml each day (Burch, 2022).
Colostomy
A colostomy is formed by bringing a part of the ileum onto the surface of the abdomen (Figure 3).
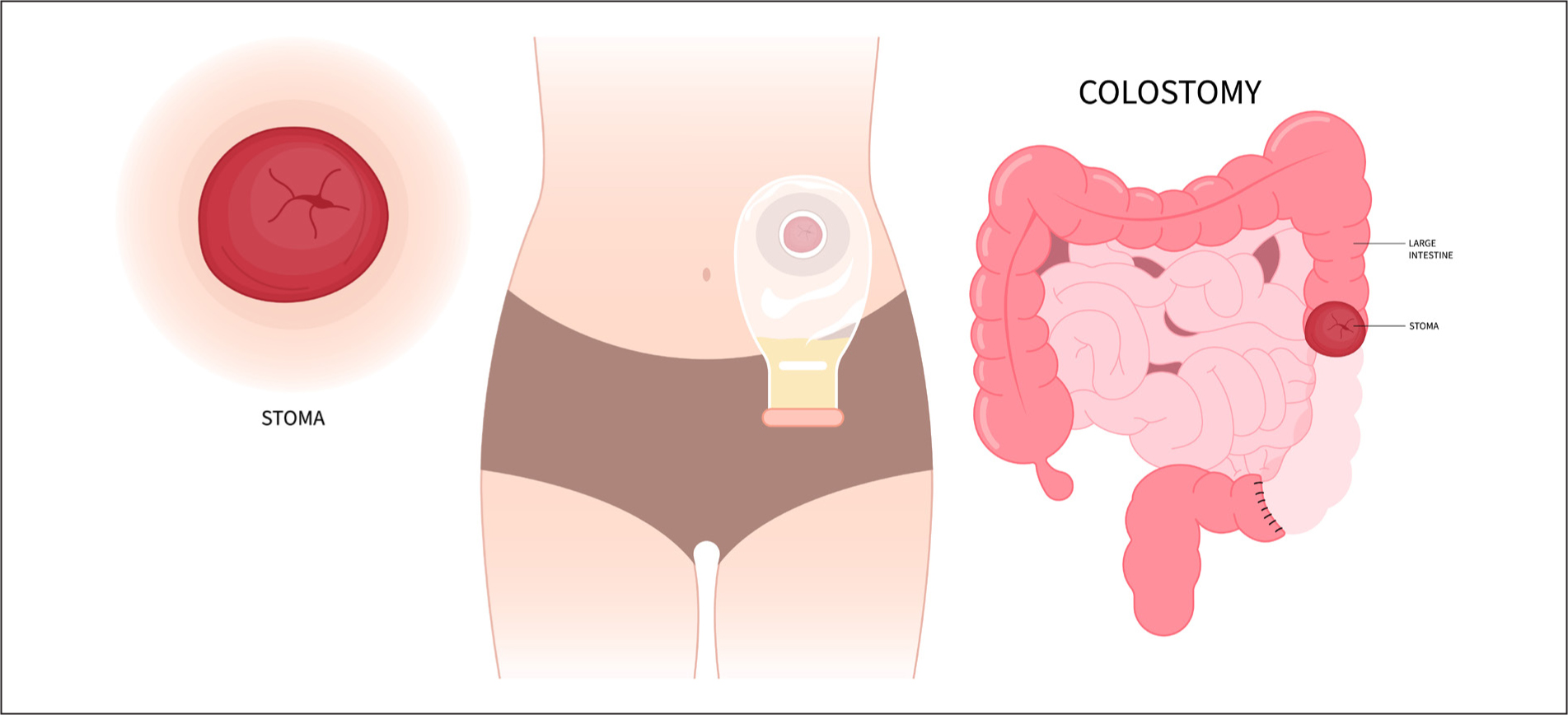
The stoma may be formed from the ascending, transverse, descending or sigmoid colon. A sigmoid colostomy and the transverse colostomy are the most usual colostomy types, whereas ascending and descending colostomies are uncommon and rarely performed. Colostomy may be carried out to treat colorectal cancers, inflammatory bowel diseases, a diverticular disease with obstruction, penetrating bowel injuries, ischemic colitis, radiation injury and as a last resort for faecal incontinence. A colostomy can be either permanent or temporary (Claessens et al, 2015).
Stomal output is related to the site of the stoma and is affected by diet and fluid intake, medication and health conditions.
Faeces produced by stomas located in the ascending colon tends to be fluid. One of the colon's functions is to absorb fluid, and faeces, which becomes more solid as it passes through the colon. Faeces produced by transverse colostomies tends to be partly formed and soft. Faeces produced by a sigmoid colostomy is formed and similar to normal faeces. Colostomy output is around 150–200 g daily (Burch, 2022).
Common problems
A large study of over 5000 people in 17 countries found that 62% of the respondents avoided physical and social activities because of their stoma and 37% had never consulted their stoma care nurse to have the fit of their stoma product checked (Martins et al, 2019). The most common problems people experience after stoma surgery are skin problems, leakage and fears about odour.
Skin problems
Peristomal skin complications are almost twice as common in people with ileostomies (Voegeli et al, 2020). Ileostomy output contains salts and digestive enzymes (proteases and lipases) and has an alkaline pH of 7.2–7.4. Ileostomy output changes the skin's acid mantle and leads to inflammation and irritation (Burch et al, 2021). The most common peristomal skin complications are moisture damage, mechanical trauma and infection. Skin problems can be caused by faeces coming into contact with the skin, the mechanical trauma of removing and replacing bags, infection and allergy (Rolstad and Erwin-Toth, 2004).
Peristomal contact dermatitis is caused by stool leaking onto the skin and causing inflammation (Figure 4). The amount of exposure as well as character of effluent will determine extent of peristomal irritation (Alvey and Beck, 2008; Ayik et al, 2020).

The incidence of peristomal skin complications varies for two reasons. The first is that there is a lack of consistent language and healthcare professionals can use different terms for the same problem. Some literature might refer to peristomal dermatitis and others to peristomal moisture-associated skin damage (PMASD). PMASD is a term used to describe any peristomal contact dermatitis predominantly caused by prolonged exposure of the skin to moisture, typically containing chemical irritants. This moisture might be perspiration and/or exudate and leakage of stool or urine from a stoma onto the surrounding skin (Burch et al, 2021). The second is that people have different operations and people vary in their ability to manage stomas.
The literature indicates that around 17–91% of people with stomas have peristomal contact dermatitis. Around 50% have PMASD, 20% maceration, 16% mechanical trauma and 1–4% infections (He et al, 2021; Singh et al, 2021).
Prevention of peristomal skin problems
Peristomal skin problems can often be prevented. Educating and enabling the individual to care for the stoma is key. Although everyone who has a stoma should be offered support from a stoma nurse, not everyone meets a stoma nurse. The person may be unwell at the time of surgery or may decline input. Sometimes, people lose touch with their stoma nurse over time. The community nurse can support the ostomate by working with the person to solve problems; the community nurse may be providing direct care or may need to refer to the stoma nurse. There are five steps to preventing peristomal skin problems, these are illustrated in Figure 5.
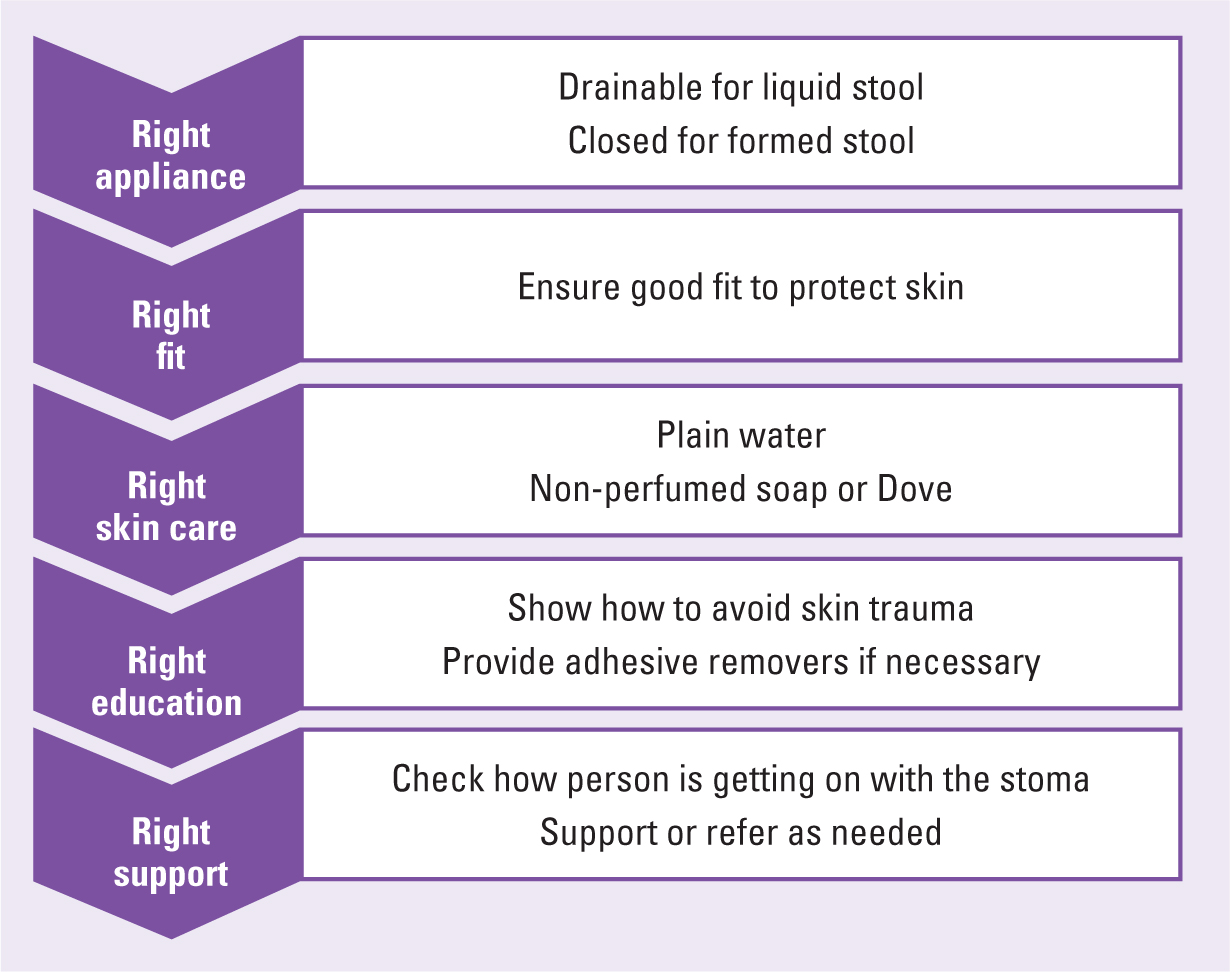
Right appliance
It is important to ensure that the person has an appropriate appliance. Stoma bags are available as drainable or closed bags, one piece or two piece and come in a variety of sizes.
The person with a sigmoid colostomy will produce around 150–200 g of formed faeces each day. A closed appliance is used in such cases; when it fills with faeces, the person removes the bag, cleans the skin and applies another. It is important to be aware that not all closed bags have flatus filters.
The person with an ileostomy will normally produce 500–800 ml of faeces daily. A drainable bag is used and the person will need to drain the bag 4–6 times a day and possibly at night. The drainable bags have a flatus filter and are folded and closed with Velcro or a clip. Ileostomy bags may be changed every 1–3 days.
The two-piece appliances consist of a base plate that sits on the skin and has a raised ridge. This clips into the bag. Some people consider two-piece appliances to be more skin friendly and others consider them more secure than a one piece bag. Other people, especially those with dexterity and visual issues, consider them fiddly and difficult to manage.
Large bags can be used if the stoma has a high output, if the person is on a long journey or requires assistance to change the bag. Small bags can be used if the person is taking part in sport or having sex (Burch, 2023).
Right fit
Leakage and fear of leakage can have a devastating effect on some people's quality of life. Around 90% of ostomates worry about leakage and 38% are very worried. Only around half of those who were very worried about leakage had sought expert help. The research did not explore the reasons why people did not seek expert help (Osbourne et al, 2022).
Leakage can occur because the bag has not been attached firmly, because flatus blows up the bag and affects the seal or because the bag is full. It is important to ensure that the skin is really dry before attaching the bag. If the skin is damp the bag will not adhere correctly.
If flatus is a problem it is important to ensure that the bag has a flatus filter; the filter enables the flatus to escape. Sometimes the amount of flatus produced can overwhelm the filter. In this case, the person with a drainable bag can drain the bag to let out the flatus. The person with a two-piece bag can release the flatus then reattach the bag. If the person has a one-piece bag, it may be necessary to change diet or change to a two-piece bag.
The person may consider changing his or her diet to reduce the amount of flatus produced. Some people find that avoiding beans, peas and onions reduces the amount of flatus. The second is to have a bag with a flatus filter.
The amount of faeces produced is dependent on the site of the stoma and the person's diet. It is important that the person uses a suitably sized bag. It is also important to ensure that the bag is changed when it is one-third full and before the person goes to bed.
If adherence continues to be a problem a number of products including adhesive paste, seals and adhesive strips can be used. Adhesive paste is a thick paste that comes in a tube. Some pastes contain alcohol and should not be used on broken skin. Adhesive strips can be moulded to improve adherence. A seal looks like a round washer and has a hole in the centre (Burch, 2023).
Right skin care
There is little evidence on the best way to care for peristomal skin and many recommendations are based on expert opinion. Soap is normally alkaline with a pH of 9-10. Skin has a pH of around 5.5 and slightly acidic. Ideally, soap would have a pH of around 5.5 and this would maintain normal skin acidity. Expert opinion recommends that plain water is used to clean the stoma and peristomal skin. If this is insufficient a mild soap is recommended. The clinician may need to be very specific about what is and what is not a mild soap.
Robertson and Brown (2011) work with cancer patients, and people having radiotherapy are advised to use ‘mild’ soap. They asked patients to identify soaps that they consider mild and tested the soaps. Patients identified Johnson's baby soap, E45, Dove, Pears, Simple soap and Imperial Leather. They tested the soaps and found that only Simple soap and Johnson's had a pH of around 5.5. All were fragranced except Simple and E45. Those that were most perfumed were Pears, Imperial Leather and Dove. In the author's experience, most people find Simple soap a little plain and do well with Dove sensitive.
It's important to stress that skin should be treated gently and patted dry.
Right education
Peristomal medical adhesive skin injuries (PMARSIs) are defined as:
‘Peristomal medical adhesive-related skin injury can be defined as an alteration in skin integrity with erythema and/or other skin alterations such as skin tears, erosion, bulla, or vesicle that is apparent after removal of an adhesive ostomy pouching system.’
PMARSIs are underresearched, underreported and underestimated (Fumarola et al, 2020). Those who are most vulnerable include older people and those with fragile skin. Le Blanc and colleagues (2019) do not recommend the routine use of adhesive remover and provide detailed guidance on how to minimise the risks of PMARSIs.
Right support
Having stoma surgery is life changing. Some people, often those who are young and who have had debilitating problems adjust well to having a stoma. Some people have pet names for their stoma. Other people can barely bring themselves to look at the stoma and need help and support. This may be practical help as the person is beginning to come to terms with the stoma and was not able to take anything in before. It might be that the person requires psychological support. If the nurse asks the person, ‘How are you getting on with your stoma?’, that helps the nurse to begin to work out what level of support the person may need and who can best provide it.
Treatment and peristomal problems
If the skin is red but intact, you can use a barrier film to protect it. Barrier films are available in sprays and wipes. The author's personal preference is to use a wipe as they believe have more control over where it is placed.
If the skin is weepy and sore you can use a stoma powder. Powders seal and protect weepy skin. They are applied to the wound and any excess can be gently brushed off (Ohura et al, 2006).
Candida albicans can cause peristomal dermatitis. Red shiny patches, papules and pustules encircle the stoma. This is treated with miconazole or clotrimazole powder (Alvey and Beck, 2008). The stoma is cleaned and patted dry, the powder is applied and excess wiped away with a cotton wool ball. A stoma film is then applied, allowed to dry and the bag is placed.
Odour
Stomas can be malodorous and some people can find this upsetting. If the bag is well-fitted and there is no leakage, then odour is only apparent when the bag is changed. There are two options to deal with malodour. The first is to use stoma deodorants and the second is to make dietary changes.
Stoma deodorants can be used to mask odour. There are two types of stoma deodorants. Some, such as nil odour are liquid and a few drops are placed in the stoma bag on changing; others such as CliniMed LiMone Deodorant Spray (which is lemon-scented) are sprayed around the room. These deodorants are very powerful and only tiny amounts are required. They can be prescribed.
The person may find that avoiding certain foods, such as cabbage and onions reduces odour. Some people find that certain foods and drinks reduce odour. Yoghurt, apples (or stewed apples) and cranberry juice can help reduce odour.
Conclusion
Many people who have stomas experience problems, yet, evidence suggests many suffer in silence and don not seek help. Problems such as sore skin, leakage and concerns about odour can have a major impact on a person's quality of life. These problems are usually easily treated and treatment makes a huge difference to the person's quality of life. By simply asking how the person is getting on with the stoma, the nurse can give the person who is experiencing problems the opportunity to get help and advice.
Key points
- Stoma surgery is life changing
- Around 62% of people with stomas avoid certain activities
- Around 38% of people do not seek help for their stoma problems
- People with colostomies may experience problems in managing it
- Common problems include skin irritation, leakage and fears about odour.
CPD reflective questions
- Mrs Brown has come to the surgery to see you. She says that she does not often get out these days, not since she had the bag. How will you explore how she is getting on and what support she might need?
- Mr Black is a 45-year-old man. He works as a sales representative and travels a lot. He has had an ileostomy and feels ‘like a new man’ after struggling for years with ulcerative colitis. He says the one problem he has is having to stop and drain the bag so often. What advice and support can you offer?


