The effects of nutrition on health have been long recognised, from James Lind conducting the first clinical trial by treating scurvy with citrus fruits in 1747 (Milne, 2012) to Korsakoff syndrome caused by thiamine deficiency most regularly associated with the long-term abuse of alcohol (Kopelman, 2022). Less commonly known is the relationship between vitamin B12 and illness, and the role it plays in supporting neurological and mental health. This article explains vitamin B12's role in mental health, and provides the background and rationale for investigating the potential role of vitamin B12 supplements in mental health.
Mental health
The World Health Organization (WHO) (2014) defines mental health as a state of wellbeing, in which an individual recognises their own potential and has the ability to cope with normal life stresses and contribute to their community. Where there is an absence of this state of wellbeing mental illness can occur, in other words a disruption to thought, behaviour, emotions, and relationships as described by the International Classification of Disease (WHO, 2022). Mental illness is one of the main causes of the overall burden of disease (Vos et al 2015), so discovering effective treatments and preventing mental health issues is important to improve people's quality of life and reduce the burden of ill health.
Vitamin B12
Vitamin B12 is the term commonly used to refer to the various chemical forms of cobalamin. It is a member of the eight co-reliant water-soluble vitamins that form the B-vitamin complex. These are essential micronutrients for the human body. This complex consists of thiamine (B1), riboflavin (B2), niacin (B3), pantothenic acid (B5), pyridoxine (B6), biotin (B7) folate (B9) and cobalamin (B12), which are required for the metabolic functions of energy conversion; lipid, protein and DNA/RNA synthesis; the myelination of neurones; and the formation of red blood cells (Green et al, 2017).
Vitamin B12 is mostly obtained in healthy humans through diet. It is produced in ruminant mammals through intestinal bacterial synthesis. Foods that are the most abundant in this vitamin are meat (especially liver), seafood, some cheeses, yeast extracts and the root nodules of legumes (peas and beans); this is mostly because of the simultaneous existence of bacteria in the soil and/or on their aerial surfaces (Azzini et al, 2021).
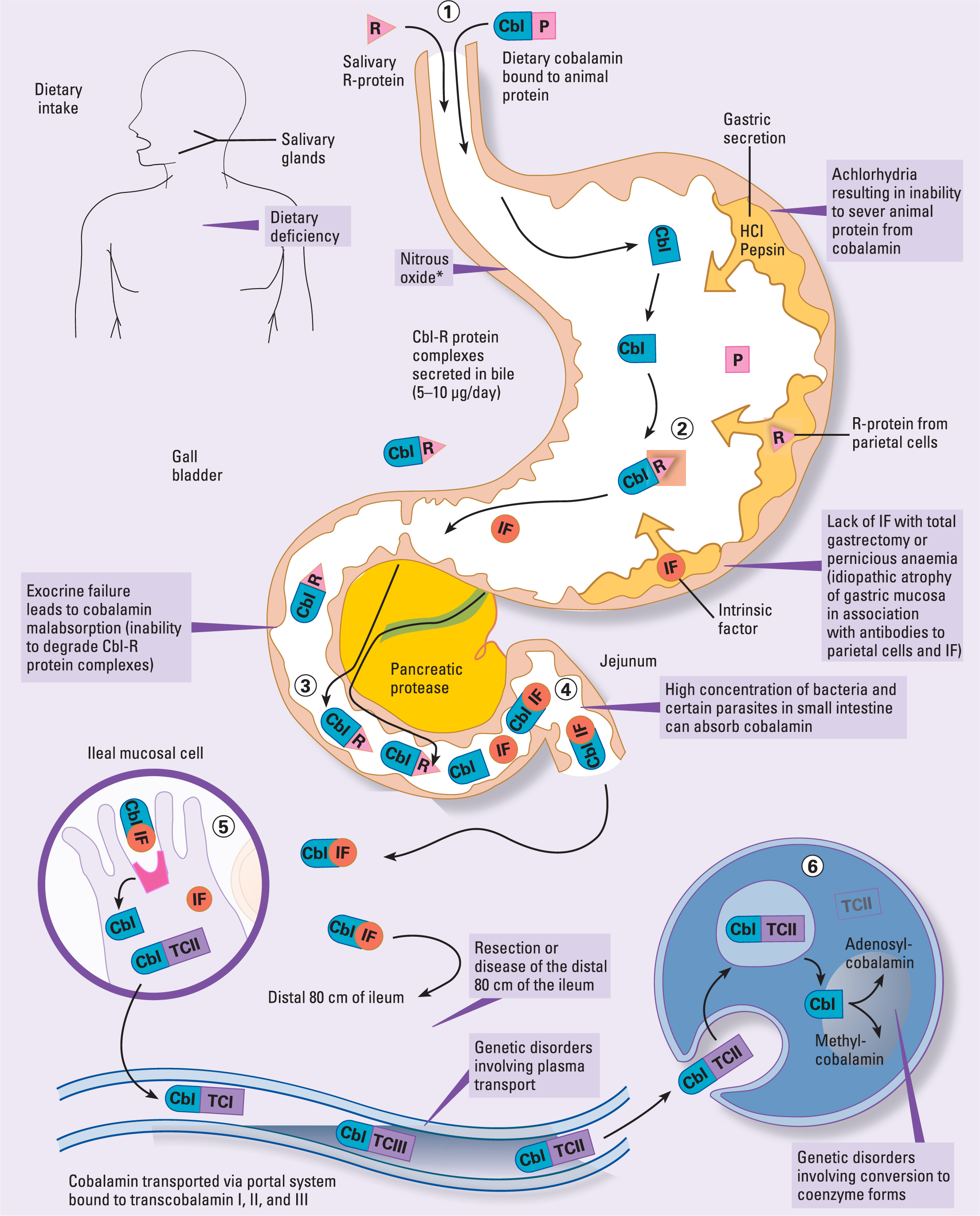
When the vitamin is available, in a healthy digestive system, hydrochloric acid and gastric protease separate the vitamin from proteins to allow the absorption of nutrients (Green et al, 2017). However, unlike other water-soluble vitamins, B12 has a unique system of absorption, delivery and activation (Figure 1), and because of this the body sometimes fails to efficiently use this nutrient (Green et al, 2017).
Low B12
Reduced intake or malabsorption of B12 can cause deficiency or sub-clinical deficiencies. It has been estimated that around 6% of people in the UK and US under the age of 60 are deficient in B12. The percentage increases to 20% in people over 60 years of age (Green et al, 2017). Over the years, the nutritional content of vitamins and minerals in fresh produced food has reduced (Thomas, 2007; Green et al, 2017), but there are additional factors in individuals that can reduce uptake of B12 or the body's ability to use it correctly.
High-risk factors
Understanding risk factors is crucial in both preventive measures and early detection of vitamin B12 deficiency. Continuous monitor ing, education and targeted interventions, especially for high-risk groups, are essential in mitigating the prevalence and adverse effects associated with low B12 levels (Green et al, 2017; McNulty et al, 2019).
It is important to note risk factors due to the high level of comorbidity that accompanies mental illness (Fiorillo and Sartorius, 2021) and the increased risk of mental illness associated with older age (Abdi et al, 2019). Ueno et al (2022) found that the neuropsychiatric manifestations of B12 deficiency can be mistaken for dementia (Table 1).
Table 1. Risk factors
| Risk factors | Comments | Authors |
|---|---|---|
| Age |
|
Green et al, 2017; McNulty et al, 2019Abdi et al, 2019; Ammouri et al, 2020 |
| Diet |
|
Green et al, 2017; McNulty et al, 2019; Falchetti et al, 2022; Fiorillo and Sartorius, 2021Kozeniecki et al, 2020; Pawlak et al, 2013; Balhara 2011 |
| Gastrointestinal disorders |
|
Green et al, 2017; McNulty et al, 2019; Ammouri et al, 2020; Keller and Layer 2014 |
| Medications |
|
Green et al, 2017; McNulty et al, 2019; Lam et al, 2013; Sobczynska-Malefora et al, 2021; Kancherla et al, 2017; Greibe et al, 2013.Ahmed et al, 2016; Damião et al, 2016Balhara 2011; Fiorillo and Sartorius, 2021Misiak et al, 2014 |
| Lifestyle |
|
Kozeniecki et al, 2020; Green et al, 2017; McNulty et al, 2019 |
| Other conditions |
|
Green et al, 2017; McNulty et al, 2019; Collins and Pawlak, 2016; Sobczynska-Malefora et al, 2021 |
| Geographic and socioeconomic |
|
Green et al, 2017 |
Why B12 is important for mental health
B12 is required for the synthesis of monoamine neurotransmitters such as serotonin and dopamine; it is required for the myelination of neurons to support the transmission of such neurotransmitters; it is also required for the methylation of homocysteine (homocysteine) which has been associated with the deterioration of brain health, linked to cognitive decline, dementias and mental illness (Türksoy et al, 2014; Olaso-Gonzalez et al, 2022). High levels of homocysteine have been found to occur more frequently in those with depression, schizophrenia (Moustafa et al, 2014; Olaso-Gonzalez et al, 2022) and obsessive-compulsive disorders (Turksoy et al, 2014). Studies have shown that supplementation of B12 at 400–1000 μg/day (166–400 µg recomended daily intake) has directly reduced the levels of homocysteine in participants by 7% with each 11% incremental rise of B12 blood serum level, without adverse effects over 12-month periods (Kennedy, 2016; Olaso-Gonzalez et al, 2022).
Psychiatric manifestations of low B12
Low levels of B12 have been known to cause psychiatric symptoms for over a hundred years; from Langdon's account in 1905 of psychiatric manifestation occurring up to 10 years before the appearance of observable biomarkers, to now where a full spectrum of psychiatric symptoms, including those often associated with psychiatric medications or psychosis, have been caused by low B12 (Victor et al, 2023). This also illustrates the risk of diagnostic overshadowing.
Around a third of B12 deficiencies are psychiatric manifestations, and over a third of hospital-admitted psychiatric patients have deficiencies of folate (an important cofactor in B12 metabolism) and B12 (Kennedy, 2016). These deficiencies occur as deficiency, sub-clinical deficiency and sub-optimal levels, as per Dhananjaya et al (2015).
The Royal College of Physicians recognises that symptoms of B12 deficiency can occur at sub-clinical levels (Shipton and Thachill, 2015), so patients could potentially be admitted or treated for mental health issues or even undergo forced treatment under the Mental Health Act (UK Parliament, 1983) as a result of no available biomarkers and blood serum levels falling within range.
Guidelines and policy
There are no UK guidelines on the therapeutic use of B12 in mental illness. The National Institute for Health and Care Excellence (NICE) recognises psychiatric manifestations of low B12 as symptoms within its guidelines for the treatment of deficiency (NICE, 2014) Methods of treatment of the deficiency require knowing the cause. Deficiency through dietary intake can be corrected through cyanocobalamin pills, but malabsorption requires high doses of hydroxocobalamin (1 mg) to be injected intramuscularly, in line with British National Formulary guidelines (Joint Formulary Committee, 2021). Symptoms of low B12 resulting from sub-clinical deficiencies are recommended to be treated only in the case of anaemia, sub-acute combined degeneration of the spinal cord or neuropathy. There are no recommendations for treating psychiatric manifestation in sub-clinical deficiency. The Joint Formulary Committee (2021) indicates using the vitamin as mentioned above or in high doses for the treatment of cyanide poisoning only.
Within the UK, there is no standardised reference range for optimal blood serum levels of B12 and there is a reliance on variable laboratory reference ranges to identify what is healthy. Being considered deficient or within normal range will depend where you live and is a ‘postcode lottery’. Therefore, there is difficulty in establishing a definition of vitamin B12 deficiency in the UK.
Rationale
There is evidence for the effects of B12 on mental health. Not only do psychiatric symptoms occur in people with low levels of B12, which people who experience mental illness are at a higher risk of developing, but B12 is also required to support neurological and brain health. It is required for the synthesis of monoamines, which need to be in correct balance to maintain balanced mental health; it is also required for the myelination of the neurones that conduct them. Vitamin B12 is a vital factor for converting damaging homocysteine and supplementing B12 has been shown to reduce this (Kałużna-Czaplińska et al, 2011). As people with mental illness have been seen to have higher levels of homocysteine, the supplementation of B12 could support the reduction of homocysteine, as well as support brain and neurological health, potentially reducing or preventing symptoms, aiding recovery and treating the risk of low levels of B12 in a low-risk and low-cost manner (Joint Formulary Committee, 2021). This literature review aims to review the evidence into this possible intervention.
Methodology
Aims and objectives
The research question, ‘can the supplementation of vitamin B12 improve mental health outcomes?’, aimed to review the research available to find evidence of whether this method of treatment could be used as independent or adjunctive psychiatric intervention (Table 2). The databases chosen for this literature review were CINAHL, Embase, MEDLINE and PsycINFO (Table 3). Advanced Boolean/phrase searches were conducted. ‘Human’ and ‘English language’ were applied as search restrictions, in line with the inclusion and exclusion criteria (Table 4).
Table 2. Definition of the PICO model, used to refine evidence based research questions
| Population/patient | People at high risk of, or with current or reoccurring mental illness or symptoms |
| Intervention | Supplementation of vitamin B12 |
| Comparison | Placebo or alternative intervention or no intervention |
| Outcome | Improvements to rates of recovery and/or relapse and prevention |
Table 3. Search terms used to identify papers
| Search Terms 1 | AND | Search Terms 2 | AND | Search Terms 3 |
| B12 | mental health | supplement* | ||
| OR | OR | OR | ||
| Vitamin B12 | mental illness | augment* | ||
| OR | OR | OR | ||
| *cobalamin | mental disorder | adjunct* | ||
| OR | ||||
| psychiatry* | ||||
| OR | ||||
| psychology* |
Note: Advanced Boolean/phrase searches were conducted with ‘human’ and ‘English language’ search restrictions applied, in line with the inclusion and exclusion criteria
*Used to broaden with search terms to retrieve variations of a term with less typing
Table 4. Inclusion/exclusion criteria
| Inclusion criteria | Exclusion criteria | Rationale |
|---|---|---|
| English language | Non-English language | Researcher's only language is English |
| Human studies | Non-human studies | Research question is focused on the human perspective |
| Studies on adult and older adults over 18 years old | Under 18 years old | The practice of mental health nursing and the improvement of mental health are non-discriminate of age |
| Geographically to include global studies | No geographical exclusions applied | Due to limited amount of research available, a wider search was conducted |
| Studies conducted between 1974-2023 | All studies available on the database were included due to the small number of relevant literatures | |
| Patients with current or past experience of, or high risk of, developing mental illness or experiencing psychiatric symptoms | People with no risk of, or current or past experience of, mental illness | Study aimed at those with experience of mental illness; this experience is required to answer research question |
| Studies administering vitamin B12 to patients | No administration of B12 to any participants | Study requires administration of vitamin B12 to answer research question |
| Primary research of randomised controlled trials | Letters, published opinions and secondary research | These research papers were best placed to directly address the question |
| Sample groups not determined by B12 status | Research to specifically treat deficiency excluding ‘normal’ B12 status participants | The aim of the study is to identify whether the addition of B12 could help all mental health patients, or only those who are classified as deficient |
| Studies that address the behavioural, emotional and perception needs of the participants | Studies that are entirely focused on improvements to the cognitive effect of dementia | Many articles produced by the databases addressed only cognitive function in those with dementia with no mention of the patient's experience of mental wellbeing |
Search results: The search, elimination process and number of results at each stage can be seen in the PRISMA (Moher et al, 2009) flow diagram below
Search results
The search and elimination process and number of results at each stage can be seen here in the PRISMA (Page et al, 2020) flow diagram (Figure 2). Five papers were identified in the final stage to be included in the literature review (Table 5).
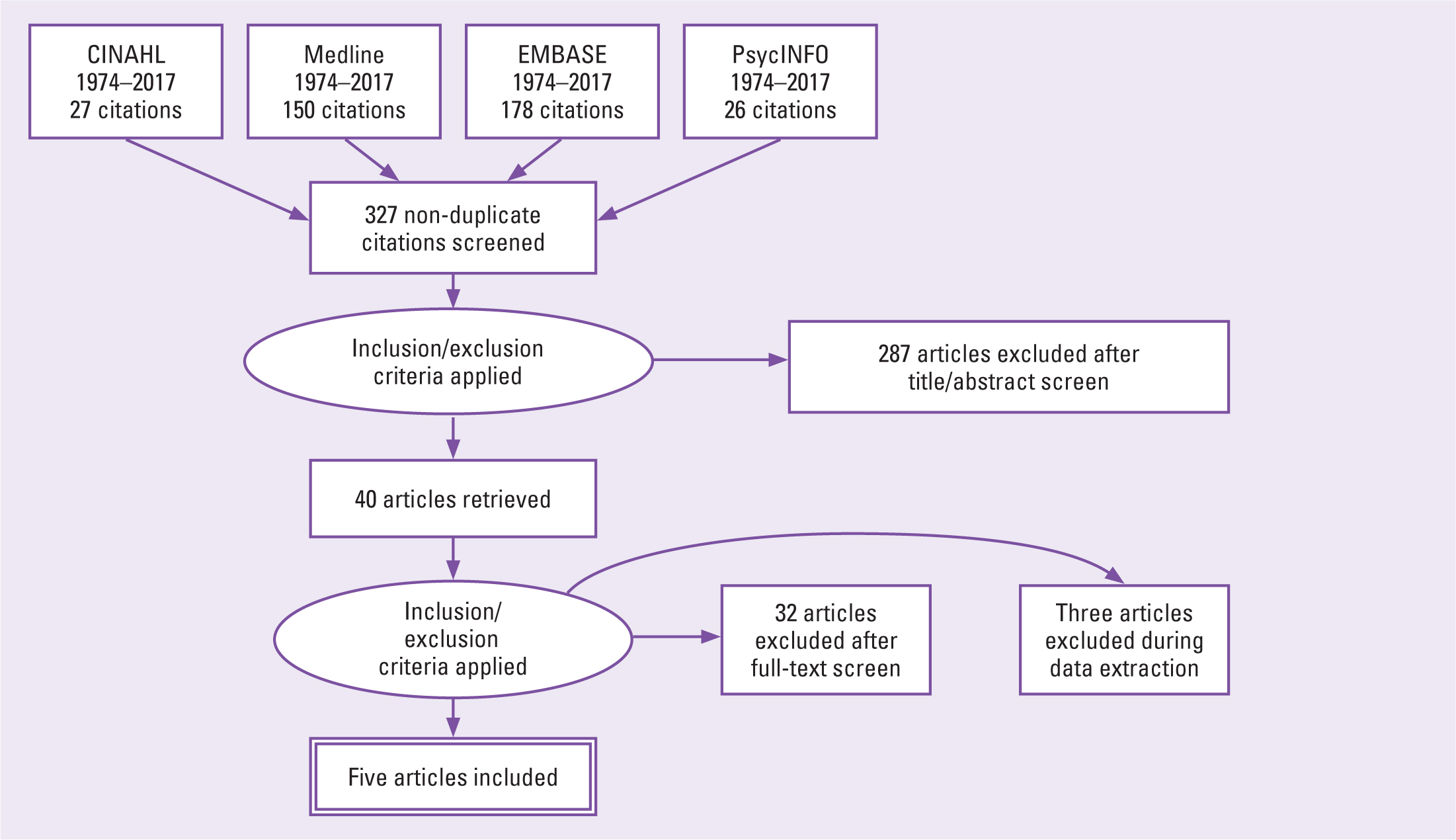
Table 5. The five papers included in this review after inclusion and exclusion criteria were applied
Findings and discussion
Overview of literature
All the papers that were returned from the search as suitable were double blind randomised controlled trials (RCT); this was non-intentional and may have been because of the search terms and criteria that were formulated from the question. None of the results returned were direct tests of the supplementation of B12 in the treatment or prevention of mental illness as a single or augmented treatment. All results returned were used in conjunction with folic acid alone or with B6 and other interventions, and were compared to placebo groups mirroring the additional intervention. There were five papers selected as addressing the research question. Each of the papers was seen to fulfil the Critical Appraisal Skills Programme's (CASP's) tool for RCTs (Singh, 2013), checklist requirements and, for the most part, fulfilled the CONSORT Statement's 25-point checklist for reporting parallel group randomised trials, thus ensuring their quality (Schulz et al, 2010).
Of the five articles, Roffman et al's (2013) study into schizophrenia was considered the strongest, followed by Almeida et al (2010). The other three studies had noticeable weaknesses and were considered to be of a lesser quality, but because B12, although among other nutrients, was considered in the studies, all articles will be discussed evenly to address the research question and the limitations considered.
Three of the final five trials were set in Australia with two of those studies (Walker et al, 2010; Christensen et al, 2011) being two separate arms of the same trial. The remaining studies were US-based (Roffman et al, 2013; Okereke et al, 2015). All the trials were outpatient or community based. All studies were conducted on older aged adults with ages ranging from 60–75 years once the trials had commenced, apart from Roffman et al (2013) in which participants were 18–68 years of age. Roffman et al's study was conducted on patients with medically stable schizophrenia and measured the effects of vitamin or B12 supplementation on reducing negative symptoms, while the remaining studies were focused on the reduction or prevention of symptoms of depression, with Christensen et al (2011) also considering the potentiation of antidepressants.
Themes
Five main themes were identified through cross-study examination: age; dose, time and vitamin forms; folate; homocysteines; and patient group specific results (Table 6).
Table 6. Main themes identified through cross-study examination of the five papers
| Themes | Almeida et al, 2010 | Christensen et al, 2011 | Okereke et al, 2015 | Roffman et al, 2013 | Walker et al, 2010 |
|---|---|---|---|---|---|
| Age | 60–74 years old | 60–74 years old | 60–74 years old | 18–68 years old | 60–74 years old |
| Dose, time and vitamin forms | ✓ | ✓ | ✓ | ✓ | ✓ |
| Folate | ✓ | ✓ | ✓ | ✓ | ✓ |
| Homocysteine | ✓ | ✓ | ✓ | ✓ | ✓ |
| Patient group specific results | ✓ | ✓ | ✓ | ✓ | ✓ |
Age
Christensen et al (2011) suggested that the lack of improvement to the participants' distress may have been due to their older age and that slowed metabolism contributed to slowed results. In contrast, Okereke et al (2015) conducted the trial into an older age sample over 10 years with still no significant effect. It is difficult to ascertain whether age can impact the effect of the treatment, as the only contrast is Roffman et al's (2013) study into schizophrenia; the sample group was of wider age range (18–68 years), but no impact on symptoms of depression was observed. However, the trial was short in comparison to the others. Evidence to support Christensen et al's (2011) hypothesis regarding older age and slowed metabolism was difficult to obtain and there was insufficient evidence to assess this. Future interventions of B12 supplementation could be measured in longer trial periods, in large sample sizes and divided into blocks of age. With the increase in the older population (Reis da Silva, 2023a; Reis da Silva, 2023b), it should be remembered that they are at a high risk of B12 deficiency, and this should be ruled out as a cause or an exacerbating factor in their mental illness.
Dose, time and vitamin forms
The trials used in cobalamin and B6 supplements are not disclosed, making it difficult to determine their effectiveness. Almeida et al (2010) found that long-term B12, folic acid, and B6 supplements could be highly effective in reducing depression in stroke survivors. However, the article lacks sufficient information for practitioners to provide an active supplement. Different types of cobalamins follow different metabolic pathways; for example, cyanocobalamin and hydroxocobalamin require conversion, whereas methylcobalamin and adenosylcobalamin are already bioavailable but have different functions within the body. Cyanocobalamin has been recorded as showing poor bioavailability and conversion rates (Scarpa et al, 2013). This could potentially raise B12 serum levels, but the body is unable to use the B12 in the blood, providing misleading blood results (higher B12 levels in the blood but giving little or no effect) (Scarpa et al, 2013). Not knowing the type of cobalamin used also restricts researchers' ability to compare the results of the trials, particularly where no effect was seen.
Any further research into the supplementation of B12 should include the form of cobalamin used, so the form itself can be assessed within the trial. This would also be important for other vitamins and minerals that may be added to the supplement.
Folate
The trials did not provide a rationale for using B12, despite its potential to reduce homocysteine (Roffman et al, 2013). Combining B12 with folic acid could mask B12 deficiency and potentially cause subacute cord degeneration and cognitive decline (Jung et al, 2015). Folic acid is not recommended for those with low B12 levels (Jung et al, 2015), and their close interrelationship makes combining them beneficial. Therefore, the use of B12 alone may not be a valid reason for its use. B12 and folate also have a tight inter-relationship, so by combining them, one can support the other (McNulty et al, 2019).
However, when using folic acid as a folate supplement there are two things to be aware of. First, folic acid is a synthetic substance formed of only minor components of folate, so the benefits of supplementing folate are not being explored when folic acid is used (McNulty et al, 2019). This undermines the research on testing the effects of folate on mental health with or without B12. Secondly, folic acid cannot pass the blood-brain barrier, so it cannot aid B12 in synthesising monoamines. Folic acid also competitively blocks the binding of natural folates to folate receptors (Olaso-Gonzalez et al, 2022), so high levels of folic acid can mask low levels of natural folates needed to support B12, potentially hindering B12 function within the brain (Olaso-Gonzalez et al, 2022). There have also been concerns around folic acid increasing the risk of cancer, so precaution should be taken when using this supplement within trials, and consideration should be made for participants whose food is fortified with folic acid through government requirement (Kim, 2008). Recommendations ask this be taken into account or that more bioavailable forms of folate be used, as was recommended by Christensen et al (2011).
Homocysteines
High levels of homocysteine being observed in those with mental illness was common rationale between the randomised controlled trials and this literature review, along with B12's ability to reduce homocysteine. By using B12 to lower homocysteine there was a rationalised possibility of reducing symptoms of mental illness. High levels of homocysteine have been found to be a precursor for mental illness (Kim and Lee, 2014). However, Almeida et al (2010), Okereke et al (2015) and Roffman et al (2013) were able to reduce homocysteine, although Almeida et al (2010) was the only study with clear results. Roffman et al (2013) showed a low level of results and significant effects for the FOLH1 genotype, but no significant result overall. Okereke et al (2015) showed no significant results of the supplementation despite the long trial period of 10.5 years. From these results, the author concludes there is no conclusive relationship between reducing homocysteine and reducing mental illness. This could contribute to further research and practice by indicating that reducing homocysteine does not necessarily reduce mental illness, and this review gives no indication that this should be method of treatment.
Patient group specific results
Despite non-significant results occurring in the majority of the literature, Almeida et al (2011) and Roffman et al (2013) did find groups that were statistically significantly helped, and whose symptoms were reduced by the supplementation of B vitamins. Both of these studies used B12 in conjunction with folic acid, and Almeida et al 2011 use B6 too. This method of treatment, particularly for stroke survivors, can reduce the burden of disease. It has the potential to reduce the cost of treatment to mental health services by preventing the need for more expensive, restrictive or harmful interventions, such as hospital admissions and use of psychoactive medications, improving quality of care and keeping to the principles of the Mental Capacity Act (UK Parliament, 2005) and the Mental Health Act (UK Parliament, 1983).
Roffman et al (2013) found that the supplement was helpful in treating negative symptoms of schizophrenia in those with the specific genotype FOLH1, because this gene affects folate metabolism. This may have been due to the folic acid supplement, but it is important to acknowledge the finding, the use of which promotes individualised, patient-centred care as required within with the Nursing and Midwifery Council's (NMC's) Code (2015).
Strengths and limitations
Apart from Christensen et al (2011) and Walker et al (2010), whose adherence measures were earlier criticised, the studies all showed a high level of adherence of 80% or more, and raised levels of the supplement proved that the groups were active. All of the studies were community based. Observations and assessments were only made at the assessment point; experiences of mood or negative symptoms relied on self-report at the assessments unless feedback had been supplied by physicians outside of the trial from no-trial treatment. This can skew the results, as their experiences are subjective. Each research team also used different assessment tools and diagnostic models for their mental health assessments, so results varied according to each. Measuring emotions and behaviours will also vary subjectively between each practitioner conducting the assessment.
Ethics
Some of the trials highlighted that for ethical reasons, people with more extreme symptoms were excluded, as were those with unstable schizophrenia and in many of the trials reviewing depression, those with major depression, bipolar or extreme levels of distress. This meant that the supplement might have been effective in the more extreme circumstances of mental illness, providing a clearer indicator for the effects of the supplement. However, because of consideration shown to these vulnerable patients in previous trials, this cannot be explored.
Adverse effects
No adverse or side effects of the supplement were observed. Roffman et al (2013) saw the relapse of 3 participants, but this was mirrored in the placebo group and was in keeping with the nature of their schizophrenia.
Has the question been answered?
This literature review examines the effects of vitamin B12 supplementation on mental health. The focus on folic acid in the papers makes it difficult to extract significant information. However, some studies suggest that B12 supplementation with folate and B6 can have positive outcomes for specific patient groups. The review suggests that there is room for development in B12's effects on mental health, but no policy or guidelines have been developed. However, practitioners could consider these outcomes for stroke patients or those with schizophrenia symptoms. This review's benefit lies in identifying areas for improvement through critical appraisal of the literature.
Limitations
The amount of evidence in relation to the research question from the literature reviewed was limited. This may reflect either the quality of the search or that information into the use of B12 in the treatment of mental illness is limited and under-researched. In retrospect, the search terms could have been extended to include treatment outside of supplementation to draw on more resources specifically aimed at the administration of B12 in mental health, or more databases could have been searched. Time constraints meant this could not be rectified. However, a systematic approach was taken in identifying the available literature to prevent bias in the selection of papers.
Conclusion
The literature that was identified in the search produced little evidence to answer the research question on B12 as a single vitamin supplement. However, the search method was structured to ensure that available evidence pertaining to the research question should have been identified and, given the articles' titles and abstracts, there was strong suggestion from preliminary searches and the systematic search conducted for this review, that there was some evidence for answering the question. The literature returned from the search showed all the studies to have been within the past seven years, suggesting this is a new area of research and that there may be little research into the effects of B12 supplementation on mental health. This review provides evidence that this is an area of research yet to be developed. This is an important finding and the detail of this review can aid the development of future research, despite not directly or conclusively answering the research question.
Key points
- Limited information on B12 supplementation as a result of focus on folic acid
- Information on B12 supplementation with folate and B6 showed no overall effect but positive outcomes for specific patient groups
- Limited research on B12's effects on mental health indicates room for development
- No policy or guidelines changed due to review
- Potential for improvement in mental health of stroke patients or schizophrenia patients
CPD reflective questions
- What is your understanding of the role of vitamin B12 in mental health?
- Based on your clinical experience, have you observed any patterns or trends regarding the relationship between vitamin B12 levels and mental health symptoms in my patients?
- How can collaboration with other healthcare professionals (eg psychiatrists, dietitians, pharmacists) enhance the effectiveness and safety of incorporating vitamin B12 supplementation into mental health treatment plans?
- What communication strategies could facilitate interdisciplinary discussions and shared decision-making regarding the use of vitamin B12 supplementation for mental health management?


